Consultations on Physician-Assisted Dying - Summary of Results and Key Findings
Annex A: Report on Issue Book Results
On February 6, 2015, the Supreme Court of Canada’s decision in Carter v. Canada held that sections 241(b) and 14 of the Criminal Code violate the constitutional rights of certain grievously and irremediably ill adult individuals. These sections of the Criminal Code currently make it illegal for anyone, including a doctor, to assist in or cause the death of another person. The Court ordered that the Criminal Code provisions remain in force for 12 months to give Parliament time to respond.
On July 17, 2015, the Government of Canada established the External Panel on Options for a Legislative Response to Carter v. Canada (the Panel) to consult with Canadians and key stakeholders on important issues relating to physician-assisted dying, such as identifying the risks and considering what rules and safeguards could look like.
This report details the results of the online consultation.
Executive Summary
Consultation Instrument – the “Issue Book”
The Panel used a public consultation methodology called the “Issue Book.” A type of workbook, the Issue Book has its roots in the field of public participation and deliberation, rather than a public opinion research survey.
Instead of simply posing questions to measure public views, the Issue Book sought to gather more informed feedback by exposing participants to background information, different perspectives on the issue of assisted dying, and fictional scenarios. The Panel used this instrument to help Canadians consider the various complex issues around assisted dying, and provide their informed input through question sets.
An advantage of the Issue Book methodology is that, by providing information and “food for thought”, it ensures participants have a basic understanding of the issue, terminology and different perspectives on the policy issue.
As a result, the Issue Book may not generate the same results as a traditional public opinion survey on the same topic. The information provided to participants is not intended to “persuade” them to respond to questions in a specific, pre-determined way.
Workbooks have been used in many online consultations in the past 15 years.
Sample Issue Book Slide: Background & Context
The Issue Book began by providing participants with factual information about the Panel, its mandate, assisted dying, and related terminology.

Description - Sample Issue Book Slide: Background & Context
Our focus: Physician assisted suicide and voluntary euthanasia
The Government of Canada needs to consider the implementation of physician-assisted dying, which is when a person seeks and obtains a medical practitioner’s help to die. There are two forms of physician-assisted dying:
- Physician-assisted suicide
- This is where patients take the final act to end their own lives, with a medical practitioner providing them with information and the means to do so. For example, they could prescribe a lethal dose of medication that patients then take to die.
- Voluntary euthanasia
- This is where a medical practitioner takes the final act that ends a patient’s life, at the patient’s request. For example, a medical practitioner could inject the patient with a lethal dose of medication.
The Carter ruling has not authorized involuntary euthanasia, which is when the patient does not request or express consent for assistance to die.
Sample Issue Book Slide: Scenarios
The Issue Book provided participants with fictional scenarios to add a “real life” dimension for consideration in responding.

Description - Sample Issue Book Slide: Scenarios
Scenario 2: Life-altering, but not life-threatening condition
Imagine that you have lost both of your legs in a serious accident. While your life expectancy has not changed, your life certainly has. You can no longer do many of the activities you enjoyed before your accident. Life feels bleak, as many of the plans you made now seem impossible. You are now considering your options.
To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die?
1- Strongly disagree-2-3-4-5 Strongly agree Prefer not to say
Sample Issue Book Slide: Safeguards
In another section, the Issue Book asked participants about safeguards while providing additional perspectives to consider by clicking “Consider…”

Description - Safeguards for Patients
How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying?
| 1 - Not important | 2 | 3 | 4 | 5 Very Important | Prefer not to say | |
|---|---|---|---|---|---|---|
| A formal written document, completed by the patient, outlining the request? Consider… | ||||||
| The presence of an impartial individual to witness the signing of the written request? Consider… | ||||||
| A repeated number of requests made by the patient? Consider… | ||||||
| A time delay between requests? Consider… |
Sample Issue Book Slide: Open-Ended Questions
The Issue Book also provided participants with an opportunity to share additional views through a series of open-ended questions at various points through the experience.

Methodology
- The online Issue Book consultation tool collected feedback on physician-assisted dying from two separate groups of the general Canadian population.
- The first group, the Open Public (“Public”), included responses from any and all individuals interested in contributing to the discourse. Responses from this group were not statistically weighted and results were more polarized on some issues.
- The second group, the online Representative Sample (“Sample”), included 2,066 responses from a representative sample of the Canadian population, weighted based on the 2011 census according to age, gender and region.
- A sample of this size is considered to be accurate within +/- 2.16% 19 times out of 20. Non-parametric tests were performed for proportions, and all statistical testing was done at a significance level of 0.05.
- The online Representative Sample group was drawn from an actively managed database (the panel) recruited by Leger, the largest Canadian-owned polling, research and strategic marketing firm.
- The Sample group panel comes from several sources: 50% are recruited randomly by Leger’s Call Centre; 35% are recruited by invitation and affiliate programs; 5% through social media; 5% by offline recruitment; and, 5% through partner programs and campaigns.
- The Leger panel is an actively managed database, and continuously tests new recruitment methods and processes.
Methodology – Use of Fictional Scenarios
At various points in the Issue Book, participants were presented with short fictional scenarios. Each explored a potential situation related to assisted dying. Participants were asked to consider the scenario and respond to a series of follow-up questions.
Scenarios are a normal workbook consultation technique, used to illustrate policy considerations to participants, showing how they might impact people in “real life.” Panel members worked carefully to develop fictional scenarios that were realistic, fair, balanced and helped participants consider the broader topic of assisted dying.
A strength of scenarios is that they enable participants to respond to concrete situations – important on a topic like assisted dying, where it may not be appropriate to consider the issue only in abstract terms. The scenarios also make it possible to observe what impact changes in context have on responses to the questions. For example, the proportion of Representative Sample respondents who strongly agree for scenario #2 drops from 13% to 6% when information is added that the event was recent.
The results for each scenario should be interpreted as a whole; by comparing responses to the overarching (first) scenario question with the relative differences in the follow-up scenario questions.
Analysis Methodology – Qualitative Data
Over 1.3 million words of qualitative data (1,368,989) were gathered from participant through the Issue Book’s open ended questions (Open Public and Representative Sample datasets). This is equivalent to over twice the word count of JRR Tolkien's “The Hobbit” and “The Lord of the Rings” trilogy combined.
This data was reviewed and formally analyzed by a team of trained qualitative researchers, coded using QSR NVivo, a specialized qualitative data analysis instrument. Data was thematically coded and placed into node structures to identify themes in participant responses. Principal themes have been summarized and example quotations identified by our researchers for inclusion in this report.
Recruitment and Outreach
The Panel’s was prevented from actively promoting its online consultation tool during the 2015 federal election period. However, the Panel did conduct an extensive public outreach campaign to over 200 Canadian organizations (including students, seniors groups, health care practitioners, etc.) to raise awareness of the online consultation. Panel members also participated in a number of media interviews (digital, print, radio and television) and made use of Panel website (ep-ce.ca) and social media tools (Twitter and Facebook) to inform Canadians on the issues and the consultation. These efforts were supplemented by a concentrated digital media advertising campaign which helped boost the number of responses to the Issue Book during the final week of the online consultation.
Eligibility
- After reviewing different scenarios, participants were generally more likely to agree physician-assisted dying should be allowed where the individual faces significant, life-threatening and/or progressive conditions. This included scenarios related to advanced dementia, challenging pain control and short-term life expectancy.
- Participants were most likely to disagree it should be allowed in scenarios related to non life-threatening conditions and situations with opportunities for rehabilitation.
Risks
- Participants were generally more concerned about risks related to mental health and patients’ emotional concerns. These include individuals requesting assistance during an episode that could be temporary, and patient’s feeling isolated or lonely.
- They were generally less concerned about implications for medical care or for risks to society, including how this would change their relationship or level of trust with their doctor.
Safeguards
- The safeguards seen to be the most important by participants included education around palliative care for providers and patients, as well as national strategies on disability supports and home care.
- While still seen as important by a majority of respondents, the safeguards less frequently identified as important largely related to procedural checks, including repeated requests by the patient, evaluation by a group of diverse professionals, consultation with others, and time delays.
Evaluation of Issue Book Questionnaire by Respondents
Respondents indicated they were very satisfied with the consultation process, particularly those from the Representative Sample:
- 90% of Representative Sample respondents and 74% of Open Public respondents agreed that “The information was clearly presented.” (2% of Representative Sample respondents and 9% of Open Public respondents disagreed)
- 87% of Representative Sample respondents and 65% of Open Public respondents agreed that “The information was well balanced between different views on the issue.” (3% of Representative Sample respondents and 16% of Open Public respondents disagreed)
- 83% of Representative Sample respondents and 61% of Open Public respondents agreed that “This online consultation helped you learn about the key issues and concerns.” (3% of Representative Sample respondents and 17% of Open Public respondents disagreed)
Who Responded
Group #1: Open Public (“Public”)
Between August 20 and November 23, 2015, the Issue Book questionnaire was completed by 12,883 Canadians. This tool was made available online (and in pdf / paper format, by request) to anyone interested, and represented some of the most active voices in the consultation.
Group #2: Representative Sample (“Sample”)
Between October 27 and November 6, 2015, a representative sample of 2,066 Canadians completed the same Issue Book questionnaire online to provide a contextual perspective, using a sample from a panel recruitment supplier.
Figure 1 - How old are you?

Figure 1 - Text equivalent
Graph charting responses to the following question: How old are you?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| Under 18 | 1% | 0% |
| 18 - 24 | 4% | 12% |
| 25 - 34 | 11% | 16% |
| 35 - 44 | 12% | 17% |
| 45 - 54 | 16% | 20% |
| 55 - 64 | 27% | 17% |
| 65 - 74 | 22% | 10% |
| 75 - 84 | 6% | 6% |
| 85 - 94 | 1% | 2% |
| 95 or older | 0% | 0% |
| Prefer not to say | 0% | 0% |
Figure 2 - What is your gender?

Figure 2 - Text equivalent
Graph charting responses to the following question: What is your gender?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| Male | 32% | 48% |
| Female | 67% | 52% |
| Prefer not to say | 1% | 0% |
Figure 3 - What province or territory do you live in?

Figure 3 - Text equivalent
Graph charting responses to the following question: What province or territory do you live in?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| British Columbia | 20% | 13% |
| Alberta | 15% | 11% |
| Saskatchewan | 3% | 3% |
| Manitoba | 7% | 4% |
| Ontario | 36% | 38% |
| Quebec | 12% | 24% |
| New Brunswick | 2% | 2% |
| Nova Scotia | 3% | 3% |
| Prince Edward Island | 0% | 0% |
| Newfoundland and Labrador | 1% | 2% |
| Yukon | 0% | 0% |
| Nunavut | 0% | 0% |
| Northwest Territories | 0% | 0% |
| Outside of Canada | 0% | 0% |
| Prefer not to say | 1% | 0% |
Figure 4 - Do you have a family doctor?

Figure 4 - Text equivalent
Graph charting responses to the following question: Do you have a family doctor?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| Yes | 92% | 86% |
| No | 7% | 14% |
| Prefer not to say | 1% | 0% |
Figure 5 - Approximately how far from your home is the nearest hospital to which you could be admitted for care?

Figure 5 - Text equivalent
Graph charting responses to the following question: Approximately how far from your home is the nearest hospital to which you could be admitted for care?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| Less than 25 km | 89% | 87% |
| 25 - 49 km | 9% | 10% |
| 50 - 99 km | 2% | 2% |
| 100 km or more | 0% | 0% |
| Prefer not to say | 1% | 0% |
Figure 6 - What do you consider to be your primary ethnic / cultural background?

Figure 6 - Text equivalent
Graph charting responses to the following question: What do you consider to be your primary ethnic / cultural background?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| White Caucasian European | 91% | 81% |
| Black African Caribbean American | 0% | 4% |
| Aboriginal First Nations Inuit Metis | 1% | 5% |
| Asian Chinese Japanese Korean | 2% | 5% |
| South Asian East Indian Pakistani | 1% | 3% |
| South or Central American | 1% | 0% |
| Other | 1% | 2% |
| Prefer not to say | 3% | 1% |
Figure 7 - Are you responding as an individual, or from a group perspective?

Figure 7 - Text equivalent
Graph charting responses to the following question: Are you responding as an individual, or from a group perspective?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| Individual | 98% | 99% |
| Group | 1% | 1% |
| Prefer not to say | 1% | 1% |
Figure 8 - Does faith play an important role in how you consider life-and-death issues?
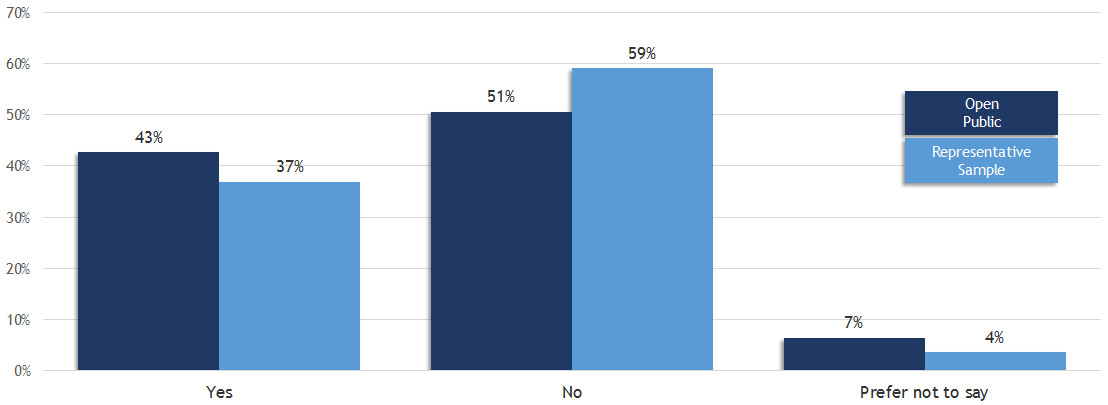
Figure 8 - Text equivalent
Graph charting responses to the following question: Does faith play an important role in how you consider life-and-death issues?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| Yes | 43% | 37% |
| No | 51% | 59% |
| Prefer not to say | 7% | 4% |
Figure 9 - Do you have a…

Figure 9 - Text equivalent
Graph charting responses to the following question: Do you have a…
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| Disability | 9% | 11% |
| Chronic disease (i.e. one that you live with every day and cannot be cured) | 20% | 16% |
| Serious or life-threatening illness (referenced as "illness" throughout report) | 4% | 3% |
Figure 10 - Are you considering / or have you considered asking for assistance to end your life (e.g. from your physician)

Figure 10 - Text equivalent
Graph charting responses to the following question: Are you considering / or have you considered asking for assistance to end your life (e.g. from your physician)
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| Yes | 15% | 9% |
| No | 81% | 88% |
| Prefer not to say | 4% | 3% |
Figure 11 - Do you work in any of these occupations / fields?

Figure 11 - Text equivalent
Graph charting responses to the following question: Do you work in any of these occupations / fields?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| Physician | 5% | 1% |
| Nurse | 9% | 2% |
| Pharmacist | 1% | 0% |
| Mental health professional | 3% | 1% |
| Social worker | 3% | 1% |
| Care or support worker | 4% | 2% |
| Other health care professional | 6% | 3% |
| Lawyer | 1% | 1% |
| Religious leader | 3% | 1% |
| Other | 27% | 33% |
Figure 12 - Do you have a family member or someone close to you with a…

Figure 12 - Text equivalent
Graph charting responses to the following question: Do you have a family member or someone close to you with a…
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| Disability | 24% | 17% |
| Chronic disease (i.e. one that he/she lives with every day and cannot be cured) | 37% | 23% |
| Serious or life-threatening illness | 21% | 10% |
Detailed Findings
Eligibility
Participants were asked to imagine how they would feel in different scenarios, to help them think through who might be eligible for assistance in dying.
Specifically, they were asked to imagine how they would feel if they were faced with each of the following diagnoses:
- Significant life-threatening illness
- Life-altering, but not life-threatening illness
- Progressive condition
- Mental health condition
Key Findings
- After reviewing different scenarios, participants were generally more likely to agree physician-assisted dying should be allowed where the individual faces significant, life-threatening and/or progressive conditions. This included scenarios related to advanced dementia, challenging pain control and short-term life expectancy.
- Participants were most likely to disagree it should be allowed in scenarios related to non life-threatening conditions and situations with opportunities for rehabilitation.
Eligibility Scenario #1: Significant life-threatening illness
Scenario Presented to Participants:
“Imagine that you have a serious life-threatening illness.
Your doctor has told you that the disease has advanced, and that you likely only have months to live.
Despite not having any significant discomfort, you are not interested in going through a long and lingering death. You are considering your end-of-life options.”
Figure 13 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die?

Among the Public, French-speaking participants, Canadians between 55 and 74, and residents of BC, ON, NB and NS were generally the most likely to agree, along with social workers and lawyers.
Among the Sample, residents of SK were less likely to agree.
Figure 13 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 37% | 14% |
| 2 | 5% | 9% |
| 3 | 5% | 17% |
| 4 | 7% | 20% |
| 5 - Strongly agree | 46% | 38% |
Figure 14 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die … if:
You could live for a few months, although there will be a challenging balance between pain control and side effects.

Among the Public, women, Canadians between 55 and 74, and residents of BC, ON, NB and NS were generally the most likely to agree, along with social workers, other healthcare professionals and lawyers.
Among the Sample, men were more likely than women to agree.
Figure 14 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die … if: You could live for a few months, although there will be a challenging balance between pain control and side effects.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 34% | 11% |
| 2 | 4% | 7% |
| 3 | 5% | 20% |
| 4 | 9% | 24% |
| 5 - Strongly agree | 47% | 35% |
Figure 15 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die … if:
Your condition may extend up to a year or two, although there will be a challenging balance between pain control and side effects.

Among the Public, Canadians between 55 and 74, and residents of BC, NB and NS were generally the most likely to agree, along with other healthcare professionals and lawyers.
Among the Sample, men were more likely than women to agree.
Figure 15 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die … if: Your condition may extend up to a year or two, although there will be a challenging balance between pain control and side effects.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 35% | 12% |
| 2 | 5% | 9% |
| 3 | 6% | 24% |
| 4 | 10% | 23% |
| 5 - Strongly agree | 43% | 29% |
Figure 16 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die … if:
Regardless of how much time you may have, you are concerned about being a burden to others, either emotionally or financially.

Among the Public, French-speaking participants, Canadians between 55 and 74, and residents of BC, NB and NS were generally the most likely to agree, along with other healthcare professionals and lawyers.
Among the Sample, responses were relatively consistent across demographic groups.
Figure 16 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die … if: Regardless of how much time you may have, you are concerned about being a burden to others, either emotionally or financially.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 41% | 18% |
| 2 | 8% | 14% |
| 3 | 9% | 20% |
| 4 | 10% | 20% |
| 5 - Strongly agree | 30% | 24% |
Figure 17 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die … if:
You received this diagnosis at the age of 16 and have a full and complete understanding of your condition and wish to die.

Among the Public, French-speaking participants, Canadians between 55 and 74, and residents of BC, NB and NS were generally the most likely to agree, along with other healthcare professionals.
Among the Sample, French-speaking participants were more likely than others to agree.
Figure 17 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die … if: You received this diagnosis at the age of 16 and have a full and complete understanding of your condition and wish to die.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 40% | 19% |
| 2 | 6% | 15% |
| 3 | 10% | 22% |
| 4 | 11% | 19% |
| 5 - Strongly agree | 29% | 21% |
Eligibility Scenario #2: Life-altering, but not life-threatening condition
Scenario Presented to Participants:
“Imagine that you have lost both of your legs in a serious accident.
While your life expectancy has not changed, your life certainly has.
You can no longer do many of the activities you enjoyed before your accident.
Life feels bleak, as many of the plans you made now seem impossible.
You are now considering your options.”
Figure 18 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die?

Broadly speaking, all demographics disagreed with this statement.
Among the Public, men, Canadians between 65 and 74, and residents of BC were generally the most likely to agree.
Among the Sample, men were generally more likely to agree in stronger terms than women.
Figure 18 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 53% | 41% |
| 2 | 12% | 18% |
| 3 | 10% | 15% |
| 4 | 7% | 11% |
| 5 - Strongly agree | 17% | 13% |
Figure 19 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die … if:
Your accident occurred five weeks ago, and you have just begun a long process of rehabilitation – at this stage you are not fully aware of the supports that might enable you to live a very good quality of life.

Broadly speaking, all demographics disagreed with this statement.
Among the Public, men, Canadians older than 65, and residents of BC and NB were generally the most likely to agree.
Among the Sample, men and Canadians under 35 were more likely than others to agree.
Figure 19 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die … if: Your accident occurred five weeks ago, and you have just begun a long process of rehabilitation – at this stage you are not fully aware of the supports that might enable you to live a very good quality of life.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 64% | 53% |
| 2 | 13% | 19% |
| 3 | 10% | 14% |
| 4 | 4% | 5% |
| 5 - Strongly agree | 8% | 6% |
Figure 20 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die … if:
Before your accident, you were a high-performance athlete and you now feel that your life has lost meaning.

Broadly speaking, all demographics disagreed with this statement.
Among the Public, men, Canadians older than 85, residents of BC and lawyers were generally the most likely to agree.
Among the Sample, men were more likely than women to agree, while Canadians between 55 and 64 were more likely to disagree.
Figure 20 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die … if: Before your accident, you were a high-performance athlete and you now feel that your life has lost meaning.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 61% | 51% |
| 2 | 13% | 19% |
| 3 | 10% | 14% |
| 4 | 4% | 6% |
| 5 - Strongly agree | 10% | 7% |
To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die … if:
Figure 21 - Your accident occurred five years ago and despite receiving excellent supports (for example, a vehicle with hand controls) you are dissatisfied with your quality of life.

Broadly speaking, all demographics disagreed with this statement.
Among the Public, men, Canadians between 65 and 74, and residents of BC and NS were generally the most likely to agree.
Among the Sample, men were more likely than women to agree.
Figure 21 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die … if: Your accident occurred five years ago and despite receiving excellent supports (for example, a vehicle with hand controls) you are dissatisfied with your quality of life.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 51% | 42% |
| 2 | 11% | 20% |
| 3 | 10% | 18% |
| 4 | 8% | 9% |
| 5 - Strongly agree | 18% | 9% |
To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die … if:
Figure 22- Your accident occurred five years ago and only minimal supports have been available, leaving you dissatisfied with your quality of life.

Broadly speaking, all demographics disagreed with this statement.
Among the Public, men, Canadians between 55 and 74, and residents of BC were generally the most likely to agree.
Among the Sample, responses were relatively consistent across demographic groups.
Graph - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die … if: Your accident occurred five years ago and only minimal supports have been available, leaving you dissatisfied with your quality of life.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 50% | 38% |
| 2 | 12% | 20% |
| 3 | 11% | 18% |
| 4 | 8% | 11% |
| 5 - Strongly agree | 18% | 10% |
Eligibility Scenario #3: Progressive condition
Scenario Presented to Participants:
“Imagine that you have just been diagnosed with Alzheimer's.
The disease will have a serious impact on your life and will worsen over time.
You have discussed your prognosis extensively with your physician, and you have a clear understanding of what lies ahead for you.
You are considering options available to you.”
Figure 23 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die?

Among the Public, Canadians between 55 and 74, and residents of BC, NB and NS were generally the most likely to agree, along with lawyers.
Among the Sample, responses were relatively consistent across demographic groups.
Figure 23 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 37% | 16% |
| 2 | 5% | 13% |
| 3 | 6% | 20% |
| 4 | 9% | 21% |
| 5 - Strongly agree | 42% | 28% |
Figure 24 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die … if:
You have minor memory loss and you cannot bear to think of your future and loss of independence.

Broadly speaking, all demographics disagreed with this statement.
Among the Public, men and residents of BC and NB were generally the most likely to agree, along with lawyers.
Among the Sample, Canadians between 55 and 74 were more likely than others to disagree.
Figure 24 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die … if: You have minor memory loss and you cannot bear to think of your future and loss of independence.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 50% | 37% |
| 2 | 12% | 22% |
| 3 | 12% | 21% |
| 4 | 8% | 10% |
| 5 - Strongly agree | 17% | 9% |
Figure 25 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die … if:
You now frequently have trouble remembering your family members’ names, sometimes forget to shut the stove off, and are occasionally found wandering down the street.
Among the Public, Canadians between 65 and 74 and residents of BC, NB and NS were generally the most likely to agree.
Among the Sample, Canadians between 55 and 64 were the most likely to disagree, while those under 25 were the least likely.
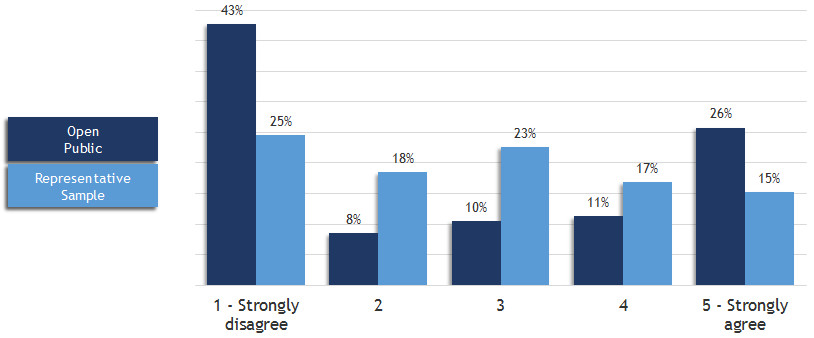
Figure 25 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die … if: You now frequently have trouble remembering your family members' names, sometimes forget to shut the stove off, and are occasionally found wandering down the street.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 43% | 25% |
| 2 | 8% | 18% |
| 3 | 10% | 23% |
| 4 | 11% | 17% |
| 5 - Strongly agree | 26% | 15% |
Figure 26 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die … if:
You now have advanced dementia and cannot make decisions on your own. However, just after your diagnosis you wrote an advance directive indicating that you would want to have a physician’s assistance to die at this stage of illness.
Among the Public, French-speaking participants, women, Canadians between 55 and 74 and residents of BC, NB and NS were generally the most likely to agree, along with social workers and lawyers.
Among the Sample, French-speaking participants were more likely than others to agree.
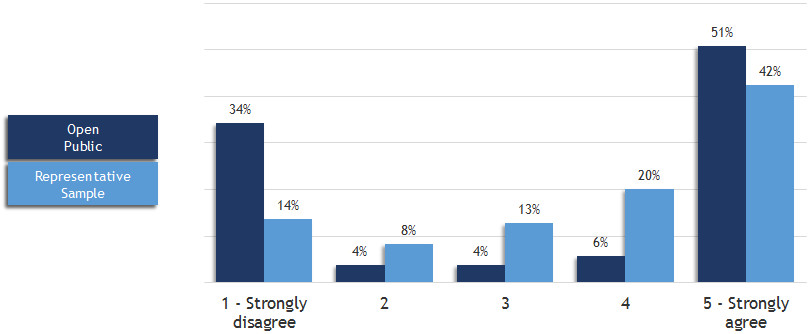
Figure 26 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die … if: You now have advanced dementia and cannot make decisions on your own. However, just after your diagnosis you wrote an advance directive indicating that you would want to have a physician's assistance to die at this stage of illness.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 34% | 14% |
| 2 | 4% | 8% |
| 3 | 4% | 13% |
| 4 | 6% | 20% |
| 5 - Strongly agree | 51% | 42% |
Eligibility Scenario #4: Mental health condition
Scenario Presented to Participants:
“Imagine that you have suffered from a mental health condition for much of your life.
Your condition has interfered with your ability to hold down steady work and has put a strain on your relationships.
You have tried many treatments, most of which did not help or caused side effects that made you want to quit.
You feel frustrated and hopeless about your future.
Despite excellent care, you are considering ending your life, but you’re afraid to try by yourself in case you don’t succeed and make things worse.”
Figure 27 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die?

Broadly speaking, all demographics disagreed with this statement.
Among the Public, Canadians between 55 and 74 and residents of BC, NB and NS were generally the most likely to agree.
Among the Sample, responses were relatively consistent across demographic groups.
Figure 27 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 45% | 31% |
| 2 | 9% | 17% |
| 3 | 10% | 20% |
| 4 | 10% | 15% |
| 5 - Strongly agree | 23% | 14% |
Figure 28 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die … if:
Your condition has worsened recently, but your physician feels that this can be helped with a change in medications.

Broadly speaking, all demographics disagreed with this statement.
Among the Public, men, Canadians older than 85 and residents of BC were generally the most likely to agree.
Among the Sample, men were more likely than women to agree.
Figure 28 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die … if: Your condition has worsened recently, but your physician feels that this can be helped with a change in medications.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 55% | 46% |
| 2 | 13% | 20% |
| 3 | 13% | 17% |
| 4 | 7% | 7% |
| 5 - Strongly agree | 10% | 7% |
Figure 29 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die … if:
You’ve been in this frame of mind before, and improved. Your condition can vary from month to month, in worse periods leaving you with suicidal thoughts.
Broadly speaking, all demographics disagreed with this statement.
Among the Public, men, Canadians older than 65 and residents of BC were generally the most likely to agree.
Among the Sample, men were more likely than women to agree.
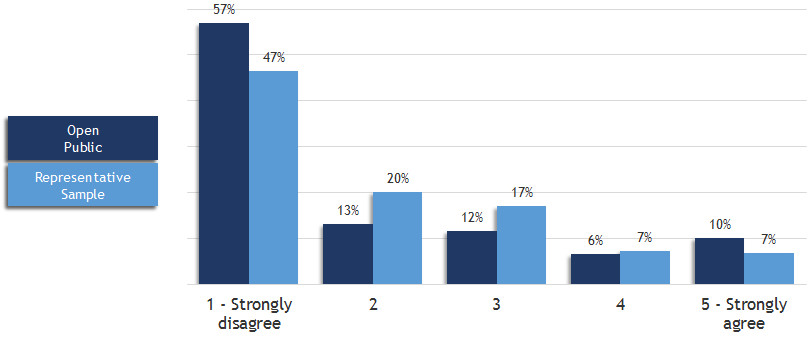
Figure 29 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die … if: You've been in this frame of mind before, and improved. Your condition can vary from month to month, in worse periods leaving you with suicidal thoughts.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 57% | 47% |
| 2 | 13% | 20% |
| 3 | 12% | 17% |
| 4 | 6% | 7% |
| 5 - Strongly agree | 10% | 7% |
Figure 30 - To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician’s assistance to die … if:
You are 17 years old, have a full and complete understanding of your condition and wish to die.

Broadly speaking, all demographics disagreed with this statement.
Among the Public, men, Canadians between 65 and 74 and residents of BC were generally the most likely to agree.
Among the Sample, men were more likely than women to agree.
Figure 30 - Text equivalent
Graph charting responses to the following question: To what extent do you agree or disagree that you (and others in this same scenario) should be able to receive a physician's assistance to die … if: You are 17 years old, have a full and complete understanding of your condition and wish to die.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 59% | 50% |
| 2 | 11% | 17% |
| 3 | 9% | 15% |
| 4 | 5% | 7% |
| 5 - Strongly agree | 12% | 9% |
Eligibility Scenarios: Strongest participant agreement
Figure 31 - Below are the five scenarios in which Public participants agreed most strongly that someone should be able to receive a physician’s assistance to die.

Note: The same five scenarios for when someone should be able to receive a physician’s assistance to die were most strongly agreed to by both Public and Sample participants (next slide).
Figure 31 - Text equivalent
Graph charting the five scenarios in which public participants agreed most strongly that someone should be able to receive a physician’s assistance to die.
| 4 Agree |
5 Strongly Agree |
|
|---|---|---|
| You now have advanced dementia and cannot make decisions on your own [but you wrote an] advanced directive that you would want to have a physician’s assistance to die | 6% | 51% |
| You could live for a few more months with your serious life-threatening condition, although there will be a challenging balance between pain control and side effects | 9% | 47% |
| Your serious life-threatening condition may extend up to a year or two, although there will be a challenging balance between pain control and side effects | 10% | 43% |
| You have a serious life-threatening illness: Your doctor has told you that the disease has advanced, and that you likely only have months to live. | 7% | 46% |
| You are diagnosed with Alzheimer's. The disease will have a serious impact on your life and will worsen over time … and you have a clear understanding of what lies ahead for you. | 9% | 42% |
Figure 32 - Below are the five scenarios in which Sample participants agreed most strongly that someone should be able to receive a physician’s assistance to die.

Figure 32 - Text equivalent
Graph charting the five scenarios in which sample participants agreed most strongly that someone should be able to receive a physician’s assistance to die.
| 4 Agree |
5 Strongly Agree |
|
|---|---|---|
| You now have advanced dementia and cannot make decisions on your own [but you wrote an] advanced directive that you would want to have a physician’s assistance to die | 20% | 42% |
| You could live for a few more months with your serious life-threatening illness, although there will be a challenging balance between pain control and side effects. | 24% | 35% |
| You have a serious life-threatening illness: Your doctor has told you that the disease has advanced, and that you likely only have months to live. | 20% | 38% |
| Your serious life-threatening condition may extend up to a year or two, although there will be a challenging balance between pain control and side effects. | 23% | 29% |
| You are diagnosed with Alzheimer's: The disease will have a serious impact on your life and will worsen over time … and you have a clear understanding of what lies ahead for you. | 9% | 42% |
Figure 33 - Below are the five scenarios in which Public participants disagreed most strongly that someone should be able to receive a physician’s assistance to die.

Note: The same five scenarios for when someone should be able to receive a physician’s assistance to die were most strongly disagreed with by both Public and Sample participants (next slide).
Figure 33 - Text equivalent
Graph charting the five scenarios in which public participants disagreed most strongly that someone should be able to receive a physician’s assistance to die.
| 2 Disagree | 1 Strongly Disagree | |
|---|---|---|
| Your life-altering but not life-threatening accident occurred five weeks ago, and you have just begun a long process of rehabilitation at this stage you are not fully aware of the supports that might enable you to live a very good quality of life. | 13% | 64% |
| Before your life-altering but not life-threatening accident, you were a high-performance athlete and you now feel that your life has lost meaning. | 13% | 61% |
| You are 17 years old, have a full and complete understanding of your mental health condition and wish to die. | 11% | 59% |
| You’ve been in this frame of mind before, and improved. Your mental health condition can vary from month to month, in worse periods leaving you with suicidal thoughts. | 13% | 57% |
| Your mental health condition has worsened recently, but your physician feels that this can be helped with a change in medications. | 13% | 55% |
Figure 34 - Below are the five scenarios in which Sample participants disagreed most strongly that someone should be able to receive a physician’s assistance to die.

Figure 34 - Text equivalent
Graph charting the five scenarios in which sample participants disagreed most strongly that someone should be able to receive a physician's assistance to die.
| 2 Disagree | 1 Strongly Disagree | |
|---|---|---|
| Your life-altering but not life-threatening accident occurred five weeks ago, and you have just begun a long process of rehabilitation at this stage you are not fully aware of the supports that might enable you to live a very good quality of life. | 19% | 53% |
| Before your life-altering but not life-threatening accident, you were a high-performance athlete and you now feel that your life has lost meaning. | 19% | 51% |
| You are 17 years old, have a full and complete understanding of your mental health condition and wish to die. | 17% | 50% |
| You’ve been in this frame of mind before, and improved. Your mental health condition can vary from month to month, in worse periods leaving you with suicidal thoughts. | 20% | 47% |
| Your mental health condition has worsened recently, but your physician feels that this can be helped with a change in medications. | 20% | 46% |
Qualitative Feedback on Additional Eligibility Factors
Summary of responses and sampling of quotes grouped by theme for Issue Book question:
- Are there any additional factors related to eligibility for physician-assisted dying that you wish to highlight? If so, please describe below.
Theme 1: Advanced health care directives
- Summary:
- Many respondents from the Open Public group mentioned that an advance health care directive to access physician-assisted dying should be honoured. Representative Sample respondents agreed. Respondents were polarized on whether a health care proxy could make such a decision if an advance health care directive was not in place. Some people were also concerned about an advance directive being misused/abused.
- Quotes:
-
“Advance care directives must be considered paramount in decision-making as these are the expressed wishes of an individual while competent.”
(Representative Sample respondent)“A person must be able to make their legal directive for physician assisted dying BEFORE they become incapable of rational decision making.”
(Open Public respondent)“An early diagnosis of Alzheimer's disease should give the patient the right to decide to end their life. There should be a written request signed before two witnesses, and the doctor assigned to the patient must be included in the steps towards aid in dying. An example is if I do not recognize anyone and have no idea of what is happening around me.”
(Representative Sample respondent in French)
Concern about misuse/abuse:
“As a retired health care professional who taught consent legislation to my colleagues, I am aware that Ontario Consent legislation is still very poorly understood and implemented by health care professionals and ever more poorly understood by the general public. I am deeply concerned about the abuse of advance directives in such an environment of benign ignorance.”
(Open Public respondent)
Health care proxy:
“If a family member with advanced dementia, or other fatal illness, doesn't have a Living Will, there should be a provision for the executor of their will, family members, or whoever holds the enduring power of attorney, to request a doctor investigate the possibility of ending their life.”
(Open Public respondent)“An individual should be able to appoint someone to make a request for assisted death if included in a legal power of attorney for personal care if they become incapacitated and unable to follow through with their own wishes to make such a request.”
(Open Public respondent)“In the scenario of Alzheimer's with an advanced directive, the power over that person’s life and timing of death should not be in someone else’s hands despite being a health proxy.”
(Open Public respondent)“For progressive illnesses, the requests must be made while the person is still able to understand the ramifications on their families, etc. Substitute decision makers should not be making these types of decisions once the person is unable to do so for themselves if they have not previously made such a request.”
(Representative Sample respondent)
Theme 2: Age restrictions
- Summary:
- While age was consistently given as a limiting factor for eligibility for physician-assisted dying, with some expressing that age should not matter, what the age restriction should be varied. In other words, at what age people should become eligible for physician-assisted dying was not clear. The predominant rationale for excluding young people was that they were incapable of truly comprehending their situation or the weight of the decision, and therefore could not properly give informed consent. Similarly many felt that a parent or other health proxy should not be able to give consent for a minor, whereas some thought that a parent or guardian should be able to approve physician-assisted dying.
- Quotes:
-
Age of eligibility:
“Anyone under the age of 18 should not have this choice. They have not experienced life enough to make this decision for themselves.”
(Representative Sample respondent)“I think the patient should be 19+ and have a full understanding of their condition.”
(Representative Sample respondent).“Children, no matter if they are an infant up until they turn 18, should not be eligible. They have not yet formed the complex thought process involved in making this decision.”
(Representative Sample respondent)“The minimum age should be over 21 years … and it should only include incurable diseases like Alzheimer's or dementia.”
(Open Public respondent in French)“Age of course is an important factor, but consider the minor who has for example a rare disease, is well aware of their prognosis and conditions (most children with rare diseases are very well informed about their disease), and wants to consider options in consultation/collaboration with their primary care giver(s).”
(Open Public respondent)
Parental consent:
“This type of decision shouldn’t be made by minors, i.e. under age 18. Their parent/guardian shouldn’t be able to make it for them. The individual would have to be 18 and capable of making the decision on their own.”
(Open Public respondent)“Age of consent should be considered. Perhaps parent/guardians would need to approve for those under the age of majority.”
(Open Public respondent)
Theme 3: Informed Consent
- Summary:
- Linked to a patient’s right to choose physician-assisted dying, respondents in the Open Public and Representative Sample groups emphasized that a person must be able to choose physician-assisted dying with a “sound mind” and all of the requisite information to make an informed decision. Some respondents felt that if the person is unable to give informed consent, that a health proxy should be able to make the decision for that person, whereas others felt that only an individual should be able to consent for oneself. Many said that mental health and depression were seen as incapacitations to an informed decision.
- Quotes:
-
“This should be a conversation between the individual and their doctor. All that should be required is informed consent.”
(Open Public respondent)“Anyone contemplating assisted suicide should, by law, have to have an interview or series of interviews with a psychologist or psychiatrist, perhaps one appointed by the courts, to ascertain the person’s ability to understand their condition and make an informed decision on the subject.”
(Open Public respondent)“As long as a person 16 years of age or over is able to understand their options and can make their decision with competence and of sound mind, there should be no further debate. However, under no circumstances should anyone be allowed to make the decision on another person’s behalf (i.e., family/guardian of a person with an intellectual, mental, physical or other disability). This decision must be made when a person is competent, of sound mind, understands their options and can give informed consent.”
(Open Public respondent)“There should be a thorough discussion with professionals and family before an individual makes the final decision.”
(Representative Sample Respondent)“A person should be terminally ill and be able to make a decision at any point in the illness. Someone who is depressed, mental health issues is not capable of making an informed decision.”
(Representative Sample Respondent)
Theme 4: Patient Choice
- Summary:
- Many respondents in the Open Public and Representative Sample groups mentioned that a patient should be able to choose physician-assisted dying (be the decision-maker) – some stating, without many other limiting factors on eligibility. Others maintained that patients should have the right to choose physician-assisted dying, given that certain eligibility criteria are met.
- Quotes:
-
“It should be the individual’s choice (with physician consultation). Adults suffering with physical ailments (cancer, ALS, Alzheimer's etc.) should have few, if any, barriers to accessing physician-assisted dying and voluntary euthanasia. Those under 18 and those struggling with mental health issues that lead them to ask for physician-assisted dying should have different criteria for eligibility. But mentally well adults should be able to make their own decision on this matter with as few hoops to jump through as possible.”
(Open Public respondent)“This should be a personal decision. An individual should have the right to determine whether or not they want to live or die. The patient is the one who has to live with their illness, day to day. No one can determine a rating of “Quality of Life” for anyone else.”
(Open Public respondent)“It’s definitely the patient who decides whether to live or die, and this should be done before they no longer have the strength to say it.”
(Open Public respondent in French)“I believe it should always be the choice of the individual, regardless of their current medical situation, to be able to end their life. It is their right. I do not believe it IS right, just that it is THEIR right.”
(Representative Sample respondent)“If your condition is terminal, you should have the right to die with dignity and stop suffering.”
(Representative Sample respondent)
Theme 5: Significant life-threatening illness
- Summary:
- That a person is both terminally ill and in intolerable pain was the most predominant factor related to eligibility for physician-assisted dying highlighted by respondents in both the Open Public and Representative Sample groups. Respondents frequently stated that a patient having “no hope” warranted the use of physician-assisted dying as a “last resort.” Progressive, degenerative conditions were often listed alongside terminal illness as a justifiable condition for eligibility. However, respondents cautioned against disability and mental health conditions (particularly depression) as reasons for physician-assisted dying.
- Quotes:
-
Both terminally ill and in intolerable pain
“A terminal diagnosis with eminent death or very brief life expectancy, accompanied by extreme pain that cannot be controlled by analgesia.”
(Open Public respondent)“I think the court made it clear: (a) you live in pain and (b) you are about to die anyway. If you have (a) and (b) together, that's the only time the person should be eligible.”
(Representative Sample respondent)
Progressive condition
“A person with a life threatening or progressive degenerative condition is already on a path toward death, which can be “hastened.” A person who is not already at risk of dying due to a medical condition should not be encouraged or supported in choosing death.”
(Open Public respondent)”My personal opinion is that only persons with severe, incurable conditions that will not improve, e.g. terminal cancer, Alzheimer’s, ALS, etc. should be considered eligible.”
(Representative Sample respondent)
Disability and mental health condition
“I feel [physician-assisted dying] should only be available to those who are seriously ill, not just having a disability but actually seriously ill and facing intolerable pain with no chance of recovery at all.”
(Open Public respondent)“I believe one should have the option of physician-assisted death in terminal and exceptional impending death but not because the person’s mental state does not feel life is worth living because of physical disabilities.”
(Representative Sample respondent)“I think it is important, as shown in your scenarios, that mental health or depression that can be fixed with medication, doesn't get confused with an illness that you are dying from.”
(Representative Sample respondent)
Theme 6: Supports and alternatives
- Summary:
- Another prominent theme that emerged from Open Public responses on factors related to eligibility for physician-assisted dying was that patients have access to palliative care, or alternative treatments (particularly for mental health), to ensure that they have considered all other options before qualifying for physician-assisted dying. Similarly, many participants indicated that it is important that patients have access to social supports and counselling, as well as financial supports so that the lack of these supports is not a factor in their decision-making. Having access to supports and alternatives before considering physician-assisted dying as a “last resort” was also a common theme in the Representative Sample group.
- Quotes:
-
Palliative care and alternative treatments
“All patients should have access to quality palliative care.”
(Open Public respondent)“There needs to be assurance that necessary care is available immediately as needed, be it mechanical, medication, and/or qualified attendant care, in order to maintain quality of life for the greatest length of time prior to termination as this will be a determining factor in maintaining dignity.”
(Representative Sample respondent)“Before suicide should be an option, I think every service for mental help and care assistance should be explored. Afterwards the decision should be up to the affected individual.”
(Open Public respondent)“Many of the people in the scenarios would benefit from better access to mental and physical health care… Along with criteria for assisted suicide, we must ensure that everyone is provided with such access.”
(Representative Sample respondent)
Social and financial supports
“It seems to me that there should be mandatory supports in place for individuals prior to making this decision, for example, social workers, religious supportive community, support groups, counseling, meeting others who face the similar conditions, palliative care professionals, transition counseling, etc.”
(Open Public respondent)“People should not feel a need to die because of their socio-economic situation, for example poverty or feeling like a burden to family.”
(Representative Sample respondent)
Risks
In its ruling on Carter, the Court recognized that there are risks involved in permitting physician-assisted dying in Canada.
This section focused on the risks for:
- Patients
- Persons with disabilities
- Persons with mental health conditions
- Palliative care
- Canadian society
Key Findings
- Participants were generally more concerned about risks related to mental health and patients’ emotional concerns. These include individuals requesting assistance during an episode that could be temporary, and patient’s feeling isolated or lonely.
- They were generally less concerned about implications for medical care or for risks to society, including how this would change their relationship or level of trust with their doctor.
Patients
How concerned are you that physician-assisted dying will pose the following risks?
Patients will be more likely to request assistance from a physician to die because…
Figure 35 - They feel pressured or influenced by their family / loved ones.

Among the Public, French-speaking participants, Canadians under 25 and residents of AB, MB and QC were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, concern generally increased for older demographics.
Figure 35 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Patients will be more likely to request assistance from a physician to die because… They feel pressured or influenced by their family / loved ones.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 21% | 13% |
| 2 | 14% | 15% |
| 3 | 14% | 21% |
| 4 | 12% | 19% |
| 5 - Very concerned | 39% | 29% |
Patients will be more likely to request assistance from a physician to die because…
Figure 36 - They feel they are an emotional burden to their family / loved ones.
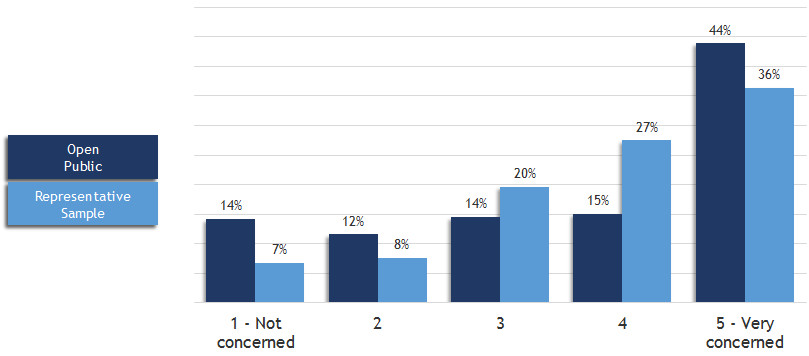
Among the Public, French-speaking participants, Canadians under 35 and residents of AB, MB and QC were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, responses were relatively consistent across demographic groups.
Figure 36 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Patients will be more likely to request assistance from a physician to die because… They feel they are an emotional burden to their family / loved ones.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 14% | 7% |
| 2 | 12% | 8% |
| 3 | 14% | 20% |
| 4 | 15% | 27% |
| 5 - Very concerned | 44% | 36% |
Patients will be more likely to request assistance from a physician to die because…
Figure 37 - They feel they are a financial burden to their family / loved ones or to society at large.

Among the Public, women, Canadians under 35 and residents of AB, MB and QC were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, concern generally increased for older demographics.
Figure 37 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Patients will be more likely to request assistance from a physician to die because… They feel they are a financial burden to their family / loved ones or to society at large.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 15% | 7% |
| 2 | 11% | 7% |
| 3 | 14% | 19% |
| 4 | 16% | 26% |
| 5 - Very concerned | 44% | 38% |
Patients will be more likely to request assistance from a physician to die because…
Figure 38 - They feel pressured or influenced by a health care provider.

Among the Public, French-speaking participants, Canadians under 25 and between 75 and 84, residents of AB, MB and QC were generally the most concerned, along with religious leaders and care or support workers.
Among the Sample, concern generally increased for older demographics.
Figure 38 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Patients will be more likely to request assistance from a physician to die because… They feel pressured or influenced by a health care provider.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 28% | 19% |
| 2 | 13% | 17% |
| 3 | 11% | 19% |
| 4 | 10% | 16% |
| 5 - Very concerned | 37% | 27% |
Patients will be more likely to request assistance from a physician to die because…
Figure 39 - They feel isolated / lonely or lack emotional support.

Among the Public, Canadians under 35 and residents of AB, MB and QC were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, responses were relatively consistent across demographic groups.
Figure 39 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Patients will be more likely to request assistance from a physician to die because… They feel isolated / lonely or lack emotional support.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 13% | 6% |
| 2 | 10% | 8% |
| 3 | 14% | 20% |
| 4 | 16% | 29% |
| 5 - Very concerned | 46% | 36% |
Patients will be more likely to request assistance from a physician to die because…
Figure 40 - They are not aware of treatments, technologies or options that might improve their quality of life.

Among the Public, women, Canadians between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians, nurses and care or support workers.
Among the Sample, Canadians between 65 and 74 were generally more concerned than others.
However, French-speaking participants were more likely than others to not be concerned.
Figure 40 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Patients will be more likely to request assistance from a physician to die because… They are not aware of treatments, technologies or options that might improve their quality of life.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 15% | 7% |
| 2 | 11% | 10% |
| 3 | 14% | 20% |
| 4 | 17% | 28% |
| 5 - Very concerned | 42% | 33% |
Patients will be more likely to request assistance from a physician to die because…
Figure 41 - They feel their health care provider doesn’t understand or provide them with other options that might address their suffering.

Among the Public, French-speaking participants, women, Canadians between 75 and 84, and residents of AB, MB and QC were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 65 and 74 were generally more concerned than others.
However, French-speaking participants were more likely than others to not be concerned.
Figure 41 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Patients will be more likely to request assistance from a physician to die because… They feel their health care provider doesn't understand or provide them with other options that might address their suffering.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 16% | 8% |
| 2 | 12% | 12% |
| 3 | 14% | 23% |
| 4 | 16% | 25% |
| 5 - Very concerned | 40% | 30% |
Patients will be more likely to request assistance from a physician to die because…
Figure 42 - They are basing their decision on an incorrect or inexact diagnosis / prognosis.

Among the Public, Canadians between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 65 and 84 were generally more likely than others to be concerned.
However, French-speaking participants were more likely than others to not be concerned.
Figure 42 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Patients will be more likely to request assistance from a physician to die because… They are basing their decision on an incorrect or inexact diagnosis / prognosis.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 16% | 8% |
| 2 | 13% | 10% |
| 3 | 14% | 22% |
| 4 | 15% | 22% |
| 5 - Very concerned | 41% | 35% |
Persons with disabilities
How concerned are you that physician-assisted dying will pose the following risks?
Persons with disabilities (and perhaps others) may be more likely to…
Figure 43 - Request assistance from a physician to die because of the suffering that arises from the experience of discrimination, deprivation or stigma.

Among the Public, French-speaking participants, Canadians under 35, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, responses were relatively consistent across demographic groups.
Figure 43 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Persons with disabilities (and perhaps others) may be more likely to… Request assistance from a physician to die because of the suffering that arises from the experience of discrimination, deprivation or stigma.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 20% | 10% |
| 2 | 15% | 15% |
| 3 | 15% | 25% |
| 4 | 13% | 23% |
| 5 - Very concerned | 36% | 24% |
Persons with disabilities (and perhaps others) may be more likely to…
Figure 44 - Be influenced to request assistance from a physician to die by a family member or caregiver upon whom they are dependent for support.

Among the Public, French-speaking participants, Canadians under 35, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more concerned than others.
Figure 44 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Persons with disabilities (and perhaps others) may be more likely to… Be influenced to request assistance from a physician to die by a family member or caregiver upon whom they are dependent for support.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 18% | 9% |
| 2 | 14% | 14% |
| 3 | 13% | 22% |
| 4 | 13% | 23% |
| 5 - Very concerned | 40% | 30% |
Persons with disabilities (and perhaps others) may be more likely to…
Figure 45 - Request assistance from a physician to die in order to be respected and admired for their sacrifice or bravery, when for much of their lives they have been devalued or ignored.

Among the Public, Canadians between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned.
However, French-speaking participants were more likely to not be concerned.
Figure 45 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Persons with disabilities (and perhaps others) may be more likely to… Request assistance from a physician to die in order to be respected and admired for their sacrifice or bravery, when for much of their lives they have been devalued or ignored.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 31% | 21% |
| 2 | 13% | 17% |
| 3 | 12% | 19% |
| 4 | 9% | 16% |
| 5 - Very concerned | 32% | 24% |
Health care providers…
Figure 46 - Being unfamiliar with other ways to address the difficulties or distress a person with disabilities is experiencing.

Among the Public, French-speaking participants, Canadians between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 45 and 54 were more likely to not be concerned.
Figure 46 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Health care providers… Being unfamiliar with other ways to address the difficulties or distress a person with disabilities is experiencing.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 22% | 11% |
| 2 | 13% | 14% |
| 3 | 13% | 23% |
| 4 | 14% | 23% |
| 5 - Very concerned | 37% | 26% |
Health care providers…
Figure 47 - Being more inclined to see requests for assistance to die from persons with disabilities as reasonable.

Among the Public, French-speaking participants, Canadians under 35, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely to be concerned, while those between 45 and 54 were more likely to not be concerned.
Figure 47 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Health care providers… Being more inclined to see requests for assistance to die from persons with disabilities as reasonable.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 24% | 11% |
| 2 | 13% | 14% |
| 3 | 12% | 25% |
| 4 | 11% | 22% |
| 5 - Very concerned | 38% | 25% |
Persons with mental health conditions
How concerned are you that physician-assisted dying will pose the following risks?
Figure 48 - A mental health condition could make it more difficult for people to receive a physician’s assistance to die.

Among the Public, French-speaking participants, Canadians between 65 and 84, and residents of QC were generally the most concerned.
Among the Sample, responses were relatively consistent across demographic groups.
Figure 48 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? A mental health condition could make it more difficult for people to receive a physician's assistance to die.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 24% | 10% |
| 2 | 10% | 9% |
| 3 | 18% | 25% |
| 4 | 19% | 30% |
| 5 - Very concerned | 23% | 23% |
Persons with mental health conditions may…
Figure 49 - Request assistance from a physician to die during an episode that could be temporary.

Among the Public, Canadians under 35, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, responses were relatively consistent across demographic groups.
Figure 49 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Persons with mental health conditions may… Request assistance from a physician to die during an episode that could be temporary.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 12% | 6% |
| 2 | 9% | 7% |
| 3 | 13% | 16% |
| 4 | 16% | 26% |
| 5 - Very concerned | 49% | 43% |
Figure Persons with mental health conditions may…
Figure 50 - Request assistance from a physician to die because of suffering / alienation that arises from the experience of discrimination, poverty, violence or stigma.

Among the Public, women, Canadians under 35, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned, while those between 45 and 54 were more likely to not be concerned.
Figure 50 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Persons with mental health conditions may… Request assistance from a physician to die because of suffering / alienation that arises from the experience of discrimination, poverty, violence or stigma.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 14% | 6% |
| 2 | 11% | 10% |
| 3 | 14% | 21% |
| 4 | 16% | 27% |
| 5 - Very concerned | 44% | 33% |
Persons with mental health conditions may…
Figure 51 - Be influenced by others in positions of authority to request assistance from a physician to die.

Among the Public, French-speaking participants, Canadians between 75 and 84, and residents of AB, MB and QC were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 65 and 84 were more likely to be concerned.
Figure 51 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Persons with mental health conditions may… Be influenced by others in positions of authority to request assistance from a physician to die.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 19% | 10% |
| 2 | 14% | 13% |
| 3 | 12% | 19% |
| 4 | 12% | 22% |
| 5 - Very concerned | 42% | 34% |
Persons with mental health conditions may…
Figure 52 - Have difficulty with the reasoning and judgment required to request a physician’s assistance to die.
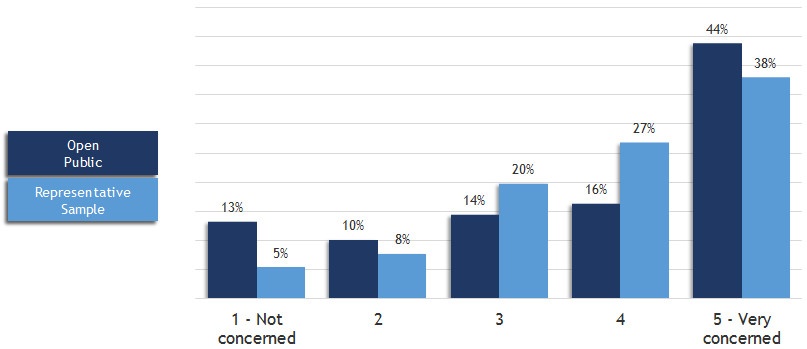
Among the Public, French-speaking participants, and residents of AB, MB and QC were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely to be concerned, while those between 45 and 54 were more likely than others to not be concerned.
Figure 52 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Persons with mental health conditions may… Have difficulty with the reasoning and judgment required to request a physician's assistance to die.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 13% | 5% |
| 2 | 10% | 8% |
| 3 | 14% | 20% |
| 4 | 16% | 27% |
| 5 - Very concerned | 44% | 38% |
Healthcare providers…
Figure 53 - May not be able to reliably assess the decision-making capacity of persons with mental health conditions.

Among the Public, women, Canadians under 35 and between 75 and 84, and residents of AB, MB and QC were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned, compared to those between 45 and 54 who were more likely to not be concerned.
Figure 53 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Healthcare providers… May not be able to reliably assess the decision-making capacity of persons with mental health conditions.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 15% | 6% |
| 2 | 12% | 8% |
| 3 | 14% | 22% |
| 4 | 17% | 29% |
| 5 - Very concerned | 40% | 33% |
Healthcare providers…
Figure 54 - May be unfamiliar with ways to address the difficulties or distress a person with mental health conditions is experiencing.

Among the Public, women, Canadians between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned, compared to those between 45 and 54 who were more likely to not be concerned.
Figure 54 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Healthcare providers… May be unfamiliar with ways to address the difficulties or distress a person with mental health conditions is experiencing.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 16% | 6% |
| 2 | 12% | 10% |
| 3 | 13% | 23% |
| 4 | 17% | 29% |
| 5 - Very concerned | 40% | 31% |
Healthcare providers…
Figure 55 - Might be less inclined to question requests for assistance to die from persons with mental health conditions.

Among the Public, French-speaking participants, Canadians between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned, compared to those between 45 and 54 who were more likely to not be concerned.
Figure 55 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Healthcare providers… Might be less inclined to question requests for assistance to die from persons with mental health conditions.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 21% | 9% |
| 2 | 13% | 13% |
| 3 | 13% | 23% |
| 4 | 14% | 25% |
| 5 - Very concerned | 37% | 28% |
Palliative care
Figure 56 - How concerned are you that physician-assisted dying will pose the following risks?
Patients will be more likely to request assistance from a physician to die because they…
Are not aware of available palliative care services.

Among the Public, Canadians between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely to be concerned than others, while those between 45 and 54 were more likely to not be concerned.
Figure 56 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Patients will be more likely to request assistance from a physician to die because they… Are not aware of available palliative care services.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 26% | 13% |
| 2 | 12% | 15% |
| 3 | 11% | 21% |
| 4 | 12% | 22% |
| 5 - Very concerned | 38% | 27% |
Patients will be more likely to request assistance from a physician to die because they…
Figure 57 - Do not have access to palliative care services and supports.

Among the Public, Canadians between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned.
Figure 57 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Patients will be more likely to request assistance from a physician to die because they… Do not have access to palliative care services and supports.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 18% | 9% |
| 2 | 10% | 10% |
| 3 | 10% | 18% |
| 4 | 13% | 25% |
| 5 - Very concerned | 47% | 35% |
Healthcare providers…
Figure 58 -Have not been trained in how to discuss palliative care options with patients.

Among the Public, women, Canadians between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned, while those between 45 and 54 were more likely to not be concerned.
Figure 58 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Healthcare providers… Have not been trained in how to discuss palliative care options with patients.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 21% | 13% |
| 2 | 12% | 15% |
| 3 | 12% | 21% |
| 4 | 15% | 24% |
| 5 - Very concerned | 38% | 26% |
Healthcare providers…
Figure 59 - Have not had the education or do not have the skills to provide effective palliative care.
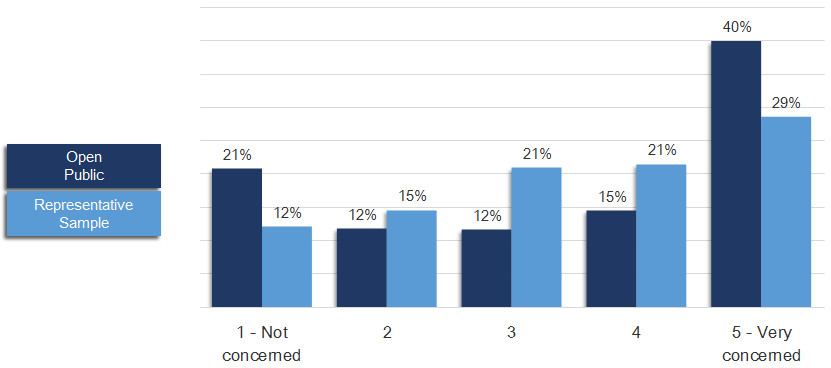
Among the Public, women, Canadians between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned, while those between 45 and 54 were more likely to not be concerned.
Figure 59 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Healthcare providers… Have not had the education or do not have the skills to provide effective palliative care.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 21% | 12% |
| 2 | 12% | 15% |
| 3 | 12% | 21% |
| 4 | 15% | 21% |
| 5 - Very concerned | 40% | 29% |
Figure 60 - Less support / resources for palliative care services across the country when assisted dying might be considered more “cost effective.”

Among the Public, women, Canadians under 35 and between 75 and 84, and residents of AB, MB and QC were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned, while residents of AB and those between 45 and 54 were more likely to not be concerned.
Figure 60 - Text equivalent
Graph charting responses to the following question: How concerned are you that physician-assisted dying will pose the following risks? Less support / resources for palliative care services across the country when assisted dying might be considered more "cost effective."
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 29% | 13% |
| 2 | 9% | 11% |
| 3 | 8% | 19% |
| 4 | 9% | 21% |
| 5 - Very concerned | 45% | 34% |
Implications for medical care
There are concerns that this could change the way some health care providers define their role and what they do, which some people worry may eventually affect how they serve their patients.
Figure 61 - How concerned are you that this would change your relationship or level of trust with your doctor?

Among the Public, men, Canadians under 25 and between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders and physicians.
Among the Sample, Canadians between 75 and 84 were more likely to be concerned.
Figure 61 - Text equivalent
Graph charting responses to the following question: There are concerns that this could change the way some health care providers define their role and what they do, which some people worry may eventually affect how they serve their patients. How concerned are you that this would change your relationship or level of trust with your doctor?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 44% | 32% |
| 2 | 10% | 15% |
| 3 | 9% | 19% |
| 4 | 8% | 14% |
| 5 - Very concerned | 28% | 17% |
Figure 62 - How concerned are you that physicians may not be aware of or do not have access to the resources needed to support patients who are considering ending their lives?
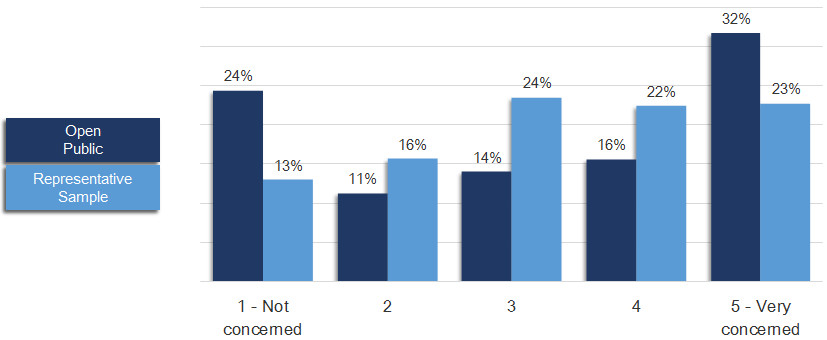
Among the Public, women and residents of AB were generally the most concerned, along with religious leaders and physicians.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned.
Figure 62 - Text equivalent
Graph charting responses to the following question: There are concerns that this could change the way some health care providers define their role and what they do, which some people worry may eventually affect how they serve their patients. How concerned are you that physicians may not be aware of or do not have access to the resources needed to support patients who are considering ending their lives?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 24% | 13% |
| 2 | 11% | 16% |
| 3 | 14% | 24% |
| 4 | 16% | 22% |
| 5 - Very concerned | 32% | 23% |
Figure 63 - How concerned are you that physicians may not be aware of or do not have access to the resources needed to facilitate requests to die from eligible patients?

Among the Public, women and Canadians between 65 and 84 were generally the most concerned.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned.
Figure 63 - Text equivalent
Graph charting responses to the following question: There are concerns that this could change the way some health care providers define their role and what they do, which some people worry may eventually affect how they serve their patients. How concerned are you that physicians may not be aware of or do not have access to the resources needed to facilitate requests to die from eligible patients?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 30% | 14% |
| 2 | 12% | 15% |
| 3 | 14% | 25% |
| 4 | 15% | 22% |
| 5 - Very concerned | 27% | 22% |
Risks to society
How concerned are you about the following issues?
Figure 64 - Normalizing societal views on assisted dying as an alternative to other ways of addressing suffering.

Among the Public, French-speaking participants, Canadians under 35 and between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned.
Figure 64 - Text equivalent
Graph charting responses to the following question: How concerned are you about the following issues? Normalizing societal views on assisted dying as an alternative to other ways of addressing suffering.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 30% | 15% |
| 2 | 11% | 13% |
| 3 | 9% | 25% |
| 4 | 7% | 20% |
| 5 - Very concerned | 42% | 24% |
Figure 65 - Negative public perceptions around the quality of life and dignity of persons with disabilities, mental health conditions or chronic health conditions.

Among the Public, French-speaking participants, women, Canadians under 35 and between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, men were more likely than women to not be concerned.
Figure 65 - Text equivalent
Graph charting responses to the following question: How concerned are you about the following issues? Negative public perceptions around the quality of life and dignity of persons with disabilities, mental health conditions or chronic health conditions.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 25% | 12% |
| 2 | 11% | 13% |
| 3 | 10% | 24% |
| 4 | 10% | 22% |
| 5 - Very concerned | 43% | 26% |
Figure 66 - Less public support / fewer resources for accommodating persons with disabilities, mental health conditions or chronic health conditions.

Among the Public, French-speaking participants, women, Canadians under 35 and between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned, while residents from MB were more likely than others to not be concerned.
Figure 66 - Text equivalent
Graph charting responses to the following question: How concerned are you about the following issues? Less public support / fewer resources for accommodating persons with disabilities, mental health conditions or chronic health conditions.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 24% | 10% |
| 2 | 9% | 11% |
| 3 | 9% | 20% |
| 4 | 11% | 23% |
| 5 - Very concerned | 46% | 33% |
Figure 67 - A decrease in public confidence in the health care system.

Among the Public, Canadians between 75 and 84, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned, while men and those between 45 and 54 were more likely than others to not be concerned.
Figure 67 - Text equivalent
Graph charting responses to the following question: How concerned are you about the following issues? A decrease in public confidence in the health care system.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 37% | 22% |
| 2 | 11% | 18% |
| 3 | 10% | 21% |
| 4 | 9% | 17% |
| 5 - Very concerned | 31% | 19% |
Figure 68 - Poverty, isolation, or social disadvantage could influence patients’ decisions to request assisted dying.

Among the Public, Canadians under 35, and residents of AB and MB were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned, while men were more likely than others to not be concerned.
Figure 68 - Text equivalent
Graph charting responses to the following question: How concerned are you about the following issues? Poverty, isolation, or social disadvantage could influence patients' decisions to request assisted dying.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 19% | 9% |
| 2 | 11% | 11% |
| 3 | 12% | 19% |
| 4 | 14% | 25% |
| 5 - Very concerned | 44% | 34% |
Figure 69 -Assisted dying could become more broadly available (for example, eligibility expanding to other groups, such as mature minors).

Among the Public, Canadians under 35 and between 75 and 84, and residents of AB, MB and QC were generally the most concerned, along with religious leaders, physicians and care or support workers.
Among the Sample, Canadians between 75 and 84 were more likely than others to be concerned.
Figure 69 - Text equivalent
Graph charting responses to the following question: How concerned are you about the following issues? Assisted dying could become more broadly available (for example, eligibility expanding to other groups, such as mature minors).
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not concerned | 30% | 14% |
| 2 | 10% | 13% |
| 3 | 9% | 20% |
| 4 | 8% | 21% |
| 5 - Very concerned | 42% | 29% |
Risks
Figure 70 - Below are the five risks Public participants were the most concerned about, in relation to physician-assisted dying:

Note: The same five risks were identified as being of most concern for both Public and Sample participants (next slide).
Figure 70 - Text equivalent
Graph charting the five risks public participants were the most concerned about, in relation to physician-assisted dying:
| 4 Concerned | 5 Very Concerned | |
|---|---|---|
| Persons with mental health conditions may request assistance from a physician to die during an episode that could be temporary | 16% | 49% |
| Patients will be more likely to request it because they feel isolated / lonely or lack emotional support | 16% | 46% |
| Persons with mental health conditions may have difficulty with the reasoning and judgment required to request a physician's assistance to die | 16% | 44% |
| Patients will be more likely to request it because they feel they are a financial burden to their family / loved ones or to society at large | 16% | 44% |
| Patients will be more likely to request it because they feel they are an emotional burden to their family / loved ones | 15% | 44% |
Figure 71 - Below are the five risks Sample participants were the most concerned about, in relation to physician-assisted dying:

Figure 71 - Text equivalent
Graph charting the five risks sample participants were the most concerned about, in relation to physician-assisted dying
| 4 Concerned | 5 Very Concerned | |
|---|---|---|
| Persons with mental health conditions may request assistance from a physician to die during an episode that could be temporary | 26% | 43% |
| Persons with mental health conditions may have difficulty with the reasoning and judgment required to request a physician's assistance to die | 27% | 38% |
| Patients will be more likely to request it because they feel isolated / lonely or lack emotional support | 29% | 36% |
| Patients will be more likely to request it because they feel they are a financial burden to their family / loved ones or to society at large | 26% | 38% |
| Patients will be more likely to request it because they feel they are an emotional burden to their family / loved ones | 27% | 36% |
Figure 72 - Below are the five risks Public participants were the least concerned about, in relation to physician-assisted dying:

Note: Four of the five risks listed above (1, 2, 3 and 5) were among the five least important risks for Sample participants (next slide) as well.
Figure 72 - Text equivalent
Graph charting the five risks public participants were the least concerned about, in relation to physician-assisted dying:
| 2 Slight Concern | 1 Not Concerned | |
|---|---|---|
| This would change your relationship or level of trust with your doctor | 10% | 44% |
| A decrease in public confidence in the health care system | 11% | 37% |
| Physicians may not be aware of or do not have access to the resources needed to facilitate requests to die from eligible patients | 12% | 30% |
| A mental health condition could make it more difficult for people to receive a physician's assistance to die | 10% | 24% |
| Persons with disabilities may be more likely to request it in order to be respected and admired for their sacrifice or bravery, when for much of their lives they have been devalued or ignored | 13% | 31% |
Figure 73 - Below are the five risks Sample participants were the least concerned about, in relation to physician-assisted dying:

Figure 73 - Text equivalent
Graph charting the five risks sample participants were the least concerned about, in relation to physician-assisted dying:
| 2 Slight Concern | 1 Not Concerned | |
|---|---|---|
| This would change your relationship or level of trust with your doctor | 15% | 32% |
| A decrease in public confidence in the health care system | 18% | 22% |
| Persons with disabilities may be more likely to request it in order to be respected and admired for their sacrifice or bravery, when for much of their lives they have been devalued or ignored | 17% | 21% |
| Patients will be more likely to request it because they feel pressured or influenced by a health care provider | 17% | 19% |
| Physicians may not be aware of or do not have access to the resources needed to facilitate requests to die from eligible patients | 15% | 14% |
Qualitative Feedback on Additional Risk Factors
Summary of responses and sampling of quotes grouped by theme for Issue Book question:
- Are there any additional risks with physician-assisted dying that have not been raised? If so, please describe below.
Theme 1: Access to Assisted Dying
- Summary:
-
Of all the top risks identified, this is the most reflective of respondents’ views in support of access to physician-assisted dying. The most significant concern related to access to assisted dying is that patients will not be able to receive assistance to die because there will be many physicians refusing to participate. In this view, many respondents took issue with a physician’s personal views impacting their access to the service, as they felt that this is “putting beliefs ahead of patients’ needs. Another issue identified by respondents is the level of bureaucracy that will be implemented for physician-assisted dying, which they fear will be too slow, arduous and excessive, leading to the system getting “bogged down” and “making it impossible” to receive assistance to die. If the process is too time-consuming and delayed, it will be especially problematic for patients who are suffering and have “no luxury for multiple options and timelines.”
Respondents were also concerned about unequal and inconsistent access to assisted dying, particularly in rural and remote communities that already experience gaps in access to health care services (e.g. palliative care). As a result, access to assisted dying will “depend on where people live”, and finding the necessary knowledge and skills – let alone willing physicians – could be particularly challenging for individuals living outside of urban areas. More broadly, some respondents also feared that access to physician-assisted dying could be limited or blocked by religious / advocacy group influence and “intimidation” of both individuals and government / politicians, which they felt is unfair as this impacts end-of-life options for everyone.
Both Open Public and Representative Sample groups highlighted the risks around access to assisted dying, although the Representative Sample respondents focused most on the impact of physicians’ beliefs in restricting access (concerns around bureaucracy and geography were not as prominent).
- Quotes:
-
“A big risk is a doctor making judgement on his religious feelings and therefore not looking after the patient according to the patient's requirements and needs. The doctors opinion on how we choose to live, die or when, should never be involved.”
(Open Public respondents)“Physicians refusing to assist patients in suicide in accordance with their own moral/religious beliefs, as is sometimes the case with abortion/contraception. This might simply lead to prolonged patient suffering.”
(Representative Sample respondents)“A major risk is that it will turn into a bureaucratic nightmare - legal in theory, but inaccessible in practice. I can imagine lengthy forms, lists of documents required, consultations required with multiple health care professionals, each of whom with a long wait list; while the patient suffers and deteriorates and ultimately is not able to access assisted suicide.”
(Open Public respondents)“Changes should be Canada wide. Patients should not have to travel to another province to get the help they want as they now have to travel to other countries.”
(Open Public respondents)“Concerned that undue influence from doctors that do not support assisted dying combined with fundamentalist religious groups and conservative politicians’ bias, the information and media coverage, preventing a healthy public discourse.”
(Open Public respondents)“We risk that external influences may be more influential than what an individual actually wants for their life.”
(Open Public respondent in French)
Theme 2: Consent and Influence Issues
- Summary:
-
Many respondents from both the Open Public and Representative Sample groups expressed concern that more patients will be directed towards physician-assisted dying because of unclear consent parameters and/or influence from other parties, which are closely connected. Many respondents were particularly worried about family influence, as some patients may be encouraged by their family to request this option, or that their family may be more willing to choose it for them if they’re unable to communicate themselves. Financial considerations (e.g. inheritance, less of a burden) were the most common rationales suggested by respondents. Some also expressed concerns with physicians, who can exert significant influence over a patient’s decision making (both for and against physician-assisted dying, depending on their beliefs).
Respondents also identified risks where a patient may not have given – or be able to provide – clear and explicit consent for a wide variety of reasons, yet may still receive assistance to die (which some suggested is occurring in other jurisdictions). As a result, there were many questions around who can provide consent on behalf of the patient, as well as whose opinion takes precedence. Family / loved ones, physicians, substitute-decision makers, and those with power of attorney were all mentioned. Additionally, some felt that there are risks with consent being provided by patients in moments of temporary distress, who may change their mind over time. It is worth noting that some respondents rejected the premise of anyone but the patient being allowed to provide consent, which they felt effectively reduces the risk of physician-assisted dying.
- Quotes:
-
“Family members may request that a patient be "put out of their misery" when in effect, it is for the convenience of the family. This could involve wanting to get at the estate of the deceased sooner, rather than waiting until nature took its course.”
(Open Public respondent)“We risk that external influences may be more influential than what an individual actually wants for their life.”
(Open Public respondent in French)“Physicians and patients have an unequal relationship. A health professional who has the upper hand might pressure a patient who may not be thinking clearly due to drugs or disease to consent to a procedure that the patient might not fully understand even in the well state. That includes consenting to be euthanized.”
(Open Public respondent)“Questionable competency of the patient requesting assistance to die.”
(Representative Sample respondent)“From my years working in Palliative Care there have been times the patient has said "I wish I could just die" but the following day they have a change of heart & are ready again to take on life whatever it has to offer. Mental health patients will have many ups & downs but are happy when their suicide attempt fails & they finally get the medical attention they require.”
(Open Public respondent)“This is a personal decision and needs to remain within the confines of the choices the individual has made, and only that person can agree to participate in any ongoing discussions, ulterior motives, or harassment from other groups or individuals to influence their decision.”
(Open Public respondent)“I think the only thing that is important is the person’s wishes. If they have made the request and they have a terminal illness, it does not matter what society thinks or the doctors think - if living in pain and having no quality of life is too much for someone to handle then they should be allowed to end it. The only person that knows what they can handle and what they cannot, is the patient and I don’t believe anyone should be allowed to second guess their feelings and wishes.”
(Representative Sample respondent)
Theme 3: Devaluing Life
- Summary:
-
According to many respondents, one of the most concerning risks of physician-assisted dying is that it will contribute to the devaluing of human life, with people’s views on the sanctity of life diminishing over time. Some feel that this practice inherently threatens human dignity, as some individuals may be stigmatized and influenced to: view their own life as hopeless / less valuable / “not worth living”, feel they are a burden to others, and “need to justify their existence.” Participants expressed particular concern for vulnerable groups, such as the elderly, people with disabilities, and people with mental health issues. As a result, many felt that physician-assisted dying will ultimately change how people view each other in Canadian society: with less compassion and perceived duty to help and care for others. Additionally, some respondents discussed the positives (e.g. personal growth, family bonding) that can come from suffering and dealing with difficult situations.
Of all the concerns identified, this contained the most references to religion and spirituality. While both Open Public and Representative Sample groups identified concerns over devaluing life, it was much more prominent among Open Public respondents. Additionally, it is worth noting that these concerns are closely linked to those articulated in another top theme – Relaxing of Eligibility Criteria.
- Quotes:
-
“We are talking about a cultural slide, a degradation of everyone's life when human beings are disposable; this will change the way we treat others in general.”
(Open Public respondent)“Human beings have the right to life simply because they are human -- this is an objectively measurable standard. When the right to life is changed to something subjective, where the right comes from possessing specific abilities or enjoying certain qualities of life that others think are necessary, then the right to life becomes violable. Such a fundamental change makes it logically impossible to draw a fixed line between those who can be killed and those who cannot.”
(Open Public respondent)“PAD emphasizes that we value some lives over others. We are saying that we agree that your life no longer has meaning and importance. Does this not undermine what it means to be Canadian?”
(Open Public respondent)“Society should be caring, not killing. We should be showing compassion to those suffering, not encouraging them to end their lives. We should be loving and kind to them and help them through their troubles. God has created humans in His image, and by taking our own life we are not showing respect for God's creation.”
(Open Public respondent)“As a society we have been conditioned to believe that suffering and pain are things to be avoided, despite the fact that many people attest to positive outcomes despite pain and suffering.”
(Open Public respondent)
Theme 4: Violating Health Care Workers’ Rights
- Summary:
-
One of the predominant risks is physicians and other health care workers being pressured or forced to participate in (as well as provide referrals for) assisted dying, even if they are conscientious objectors due to moral, ethical and religious reasons. As a result, there is concern that physicians and others will effectively lose their conscience rights, as their right to refuse the practice may not be heard, respected, or legally protected (there are many questions about how this will work). Respondents felt that this is a significant burden to place on health care workers, especially since they are trained and feel obligated to protect life. Many insisted that these rights must be defended, as physicians and others need the freedom to follow their own conscience and values. There is also the fear that physicians will be discriminated against or punished if they refuse to participate, such as through fines, suspension, dismissal, and loss of their right to practice. As a broader point, some feel that physician-assisted dying will lead to a decline in health care professionals over time, as physicians could start leaving their practices and individuals may be discouraged to enter the field altogether.
Both Open Public and Representative Sample groups highlighted these risks, although it was more prominent (in relation to other identified issues) among Open Public participants. It is also worth noting that some – though far less – Open Public respondents expressed the opposite view: physicians should not be allowed to deny assisted dying due to their personal beliefs.
- Quotes:
-
“I am concerned with the pressures that will be placed on Doctors who have moral objections to this issue and the possibility that they may be legally forced to assist with assisted suicide, if they wish to keep their careers and practices. It should not be a mandatory service they must provide.”
(Open Public respondent)“Ensuring the freedom of conscience on this issue for health care providers.”
(Open Public respondent in French)“Health care providers made an oath to 'cause no harm', there will be physicians who will not want to assist in killing their patients, and will not give a referral to a doctor who will. These doctors should have the right to refuse to help their patients kill themselves.”
(Open Public respondent)“An incredible burden to place on physicians whether or not they want to assist in the death of their patient - guilt all around.”
(Open Public respondent)“Physicians who do not want to participate in assisted-suicide in any form need legal protection. They need to be able to remain in good-standing and suffer no legal / social / financial penalties.”
(Open Public respondent)“Safe-guarding the practice without any discrimination of the physician who is opposed to assisting a patient who has expressed a desire to die; and also safe-guarding the practice without any discrimination of the physician who is opposed to referring such patient to a doctor who is willing to assist a patient who has expressed a desire to die.”
(Representative Sample respondent)
Theme 5: Insufficient Training and Professionalism
- Summary:
-
Another of the top prevailing risks, respondents emphasized the need to ensure relevant education and training for physicians and other health care professionals in the area of assisted dying. Respondents noted that many physicians are not well informed of the full range of palliative / end-of-life care options more generally, let alone being prepared to effectively handle assisted dying (some indicated that the former is an important foundation / precursor to the latter). Physicians also need training to improve their communications skills in order to effectively assess, inform and discuss assisted dying with their patients. On this note, respondents also expressed concerns with how a physician’s personal traits (e.g. lack of empathy) – combined with their personal beliefs and attitudes – may negatively influence how they inform and counsel discussions around assisted dying. Considering these factors, some respondents worried about the overall subjectivity involved: while some doctors will be well equipped to deal with assisted dying, there are many who will not.
More broadly, some respondents also felt that assisted dying degrades the integrity of medical professions and may change perspectives on the patient-provider relationship, as it conflicts with the notion of providing health care, healing, and saving lives. Many respondents suggested that it should not be one physician who decides whether a patient receives assistance to die because it is “too big of a responsibility”. Multiple physicians, a team of health care professionals, or specialists in the area should be involved or provide support. While both Open Public and Representative Sample groups identified these concerns as top risks, the latter group was less explicit about the need for education and training.
- Quotes:
-
“All health care professionals need additional training to better discuss a full range of options from full aggressive treatment all the way to natural or assisted death. This should be a core skill of all health care providers to ensure patients are well informed.”
(Open Public respondent)“Health care providers do not yet have mandatory training and/or protocols around palliative care. Why would physician-assisted dying protocols and training be introduced before physicians have had compulsory training in palliative care, which is aimed at relieving suffering?”
(Open Public respondent)“Different doctors have very different skills sets when it comes to bedside manners. I would hate to think that patients' choice to end their lives could be so dependent on the way in which the "choice" pros and cons are laid out by their doctor. Some doctors could have a higher "death rate" associated with the patients under their care because of the doctor's own personal beliefs and attitudes.”
(Open Public respondent)“Doctor personal bias towards ending lives. Some doctors currently push their own personal bias towards ending life on the elderly and will refuse treatment and downgrade dnr levels on their own.”
(Representative Sample respondent)“A doctor is trained to preserve life wherever that is possible to ask them to participate in assisting suicide is a negation of that training.”
(Open Public respondent)“As a nurse I'm concerned that schools of medicine and current physicians are either not adequately trained or comfortable with breaching these topics with their patients. In addition I feel this should be approached with the idea of a team approach in mind. One in which, not only the physician, but also the patient, clergy, social worker , nurse, family, physio, psychiatrist etc. is involved in approaching the subject but also carrying out the wishes of the patient.”
(Open Public respondent)
Theme 6: Relaxing of Eligibility Criteria
- Summary:
-
There are concerns that the introduction of physician-assisted dying in Canada could lead to the eligibility criteria broadening or relaxing over time, resulting in a “slippery slope” (a term used by many respondents) where the practice normalizes and becomes more common. Respondents are worried that more individuals will become eligible to receive assistance to die, and it will become more difficult to determine who qualifies (e.g. how to quantify suffering). Respondents were most concerned about children and the elderly (especially with the aging population in Canada), but also for individuals with mental health issues, illnesses, and disabilities. Many participants warned that eligibility has broadened and assisted dying continues to increase in other jurisdictions where the practice is permitted – particularly the Netherlands. Additionally, some felt that this will also allow for greater abuse and unintended use of the practice overall. For example, there are worries that financial / economic considerations could influence decisions around assisted dying, with people being pressured to make requests because they feel they are a burden to their family / loved ones or society more broadly.
While these risks were identified by both Open Public and Representative Sample groups, it was much more prominent with the former (and is closely tied to another top theme – Devaluation of life). Overall, this was not one of the top risks highlighted by Sample respondents.
- Quotes:
-
“I am concerned that as time passes the boundaries will disappear and assisted death would be society's answer to difficult people. As soon as we open these doors others find a way to abuse the rules.”
(Open Public respondent)“How to counter the illusion that assisted dying is a solution that will quickly become the answer, because people in general are terribly afraid of suffering.”
(Open Public respondent in French)“There is not a jurisdiction in the world that has been able to successfully respond to the inherent risks with assisted suicide and euthanasia. In fact, peer-reviewed studies show that the number of physician-assisted deaths continue to increase in these other jurisdictions, even in the face of clear evidence that the law is not being properly followed.”
(Open Public respondent)“Being of Dutch background, I know that in a very short period of time, a person can ask to be euthanized for almost any reason he or she gives. Also, those who are a "burden on society" will feel the need to justify being an expense, not only to the medical care, but also to society as a whole i.e., special education programs in schools. But above all, God has created humanity in His image. We have always been taught that it is not right to murder or to kill another human being. If we cross this line, where do we end? What ground will Society stand on? I would think it will be a shifting ground.”
(Open Public respondent)“Rather than society viewing the disabled, elderly and dying with respect and compassion, they will be viewed more in terms of a burden on their family and taxpayers and considered selfish unless they seek to end their life (do the honourable thing).”
(Open Public respondent)
Theme 7: Trust in Providers and Health care System
- Summary:
-
Many respondents felt that the patient-physician relationship will ultimately change as a result of this practice. They suggested that there will be a significant shift in the physician’s role (e.g. “from caregiver / healer to death facilitator”, “from lifesaving and suffering alleviation to death providing”, “and not as a caring human being”), which will erode patient’s trust and confidence. Respondents identified various ways in which a physician’s approach, motives, and interests could direct patients toward assisted dying in various ways (e.g. feel it is more expedient than long-term care, do not have knowledge of solutions / options, want to be alleviated from being overworked or dealing with a difficult patient). Over time, they feel that more doctors will become desensitized to assisted dying and more likely to suggest it to their patients. It is worth noting that many of these respondents signalled an overall distrust or fear of health care providers and the system, with some citing negative personal experiences. In their view, the introduction of physician-assisted dying amplifies this lack of trust because it gives physicians even more power and authority over patients.
Additionally, some respondents expressed distrust in the health care system more broadly. Given the context of rising costs, significant resource constraints and an aging population, they felt that assisted dying may increasingly be seen as an economic solution for patient care. Both Open Public and Representative Sample groups expressed these concerns but it was more prominent with the Representative Sample.
- Quotes:
-
“If a doctor brought up the idea of euthanizing me with me, I would never speak to him again. I shouldn't have to die because I have a condition, and no one should ever think that. Worse, he may bring it up with family/loved ones, or they may bring it up with him. I want my doctor to try to save my life and not end it.”
(Open Public respondent)“Thus fundamentally changes the role if healthcare from a professional striving to enhance quality of life to one making decisions regarding prematurely ending life. This paradigm shift reduces the "helping", "caring" aspects of healthcare and will create a generation if health professionals who will have less regard for working with patients to find viable options to work through challenging situations to healthcare providers who gently encourage end of life as a viable option when life us hard.”
(Open Public respondent)“Considering the low qualification of many doctors in this country, and the pressure to reduce costs with health care, my concern is that euthanasia be sold as a solution to keep patient's dignity, or as an act of bravery. There's a lot of brainwashing in this country towards making people believe the most cost effective practices are in fact the best practices for the patients. Euthanasia can be seen as a "normal" solution, and be sold as a right of the patient, and even be extended to other non-life threatening situations (such as people suffering from major depression).”
(Representative Sample respondent)“In the context of budget cuts, health care professionals can be completely overwhelmed. They can be tempted to “cut corners” and go a little too fast when making these decisions.”
(Open Public respondent in French)“The medical system will always lean heavily on the side of Physician-assisted suicide because in the long run it will be much cheaper and cost effective solution to help someone die rather than support them through palliative care.”
(Open Public respondent)
Safeguards
The Court recognized that health risks cannot be completely eliminated, because they are “part and parcel of our medical system”. However, safeguards can help minimize these risks. This section focused on the safeguards for:
For certain elements, an optional pop-up box provided additional information for participants to consider when their mouse clicker hovered over a “Why” button. Reading the pop-up box was not required and some participants may have decided against doing so before responding to the question.
Key Findings
- The safeguards seen to be the most important by participants included education around palliative care for providers and patients, as well as national strategies on disability supports and home care.
- While still seen as important by a majority of respondents, the safeguards less frequently identified as important largely related to procedural checks, including repeated requests by the patient, evaluation by a group of diverse professional, consultation with others, and time delays.
Safeguards for Patients
How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying?
Figure 74 - Extensive discussion with the patient’s physician.

Among the Public, women, Canadians between 25 and 34, and residents of NL were generally more likely to find this to be very important, along with physicians and nurses.
Among the Sample, women and Canadians between 55 and 84 were more likely than others to find this important.
Figure 74 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying? Extensive discussion with the patient's physician.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 2% | 1% |
| 2 | 1% | 2% |
| 3 | 4% | 7% |
| 4 | 7% | 12% |
| 5 - Very important | 80% | 75% |
Figure 75 - Patients understand and appreciate all palliative and medical care options or supports and services (e.g. psychologist, social worker, pastoral care, medical devices, community support) that might address a patient’s suffering.
Why?
It is possible that sometimes a person’s suffering is less directly related to their medical condition and more about not having their support needs met.

Among the Public, English-speaking participants, women, Canadians between 25 and 34, and residents of AB, MB and NL were generally more likely to find this to be very important, along with most professions besides lawyers.
Among the Sample, women and Canadians between 55 and 74 were more likely than others to find this important.
Figure 75 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying? Patients understand and appreciate all palliative and medical care options or supports and services (e.g. psychologist, social worker, pastoral care, medical devices, community support) that might address a patient's suffering. Pop-up box "Why?": It is possible that sometimes a person's suffering is less directly related to their medical condition and more about not having their support needs met.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 2% | 1% |
| 2 | 1% | 1% |
| 3 | 3% | 6% |
| 4 | 7% | 13% |
| 5 - Very important | 83% | 76% |
Figure 76 - Referral to a medical specialist for a second opinion on the patient’s condition, treatment and prognosis.

Among the Public, women, Canadians between 25 and 34, and residents of AB and MB were generally more likely to find this to be very important, along with religious leaders, care or support workers and physicians.
Among the Sample, women and Canadians between 55 and 74 were more likely than others to find this important.
Figure 76 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying? Referral to a medical specialist for a second opinion on the patient's condition, treatment and prognosis.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 5% | 2% |
| 2 | 3% | 2% |
| 3 | 8% | 9% |
| 4 | 12% | 17% |
| 5 - Very important | 68% | 67% |
Figure 77 - The option of physician-assisted dying can only be discussed if the patient raises it first.
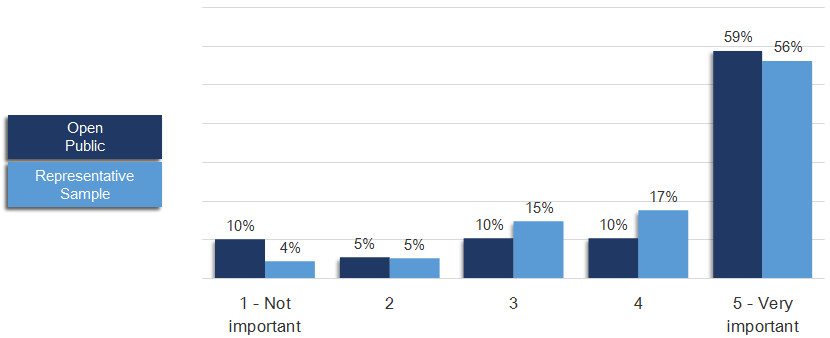
Among the Public, women and residents of AB, MB and QC were generally more likely to find this to be very important, along with religious leaders and care or support workers.
Among the Sample, women were more likely than men to find this important.
Figure 77 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying? The option of physician-assisted dying can only be discussed if the patient raises it first.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 10% | 4% |
| 2 | 5% | 5% |
| 3 | 10% | 15% |
| 4 | 10% | 17% |
| 5 - Very important | 59% | 56% |
Figure 78 - A time delay between the diagnosis of condition or injury and when a request can be considered.
Why?
This could provide patients, who may be vulnerable, time to adjust to a new reality. On the other hand, imposing a delay may seem unfair and arbitrary, since we all experience suffering differently.
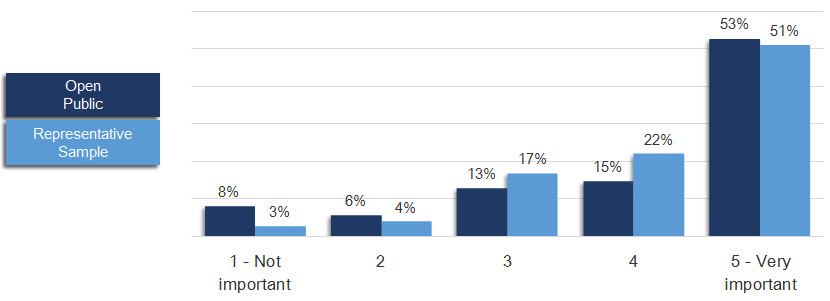
Among the Public, women and residents of AB and MB were generally more likely to find this to be very important, along with religious leaders, care or support workers and physicians.
Among the Sample, women and Canadians between 65 and 74 were more likely than others to find this important.
Figure 78 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying? A time delay between the diagnosis of condition or injury and when a request can be considered. Pop-up box "Why?": This could provide patients, who may be vulnerable, time to adjust to a new reality. On the other hand, imposing a delay may seem unfair and arbitrary, since we all experience suffering differently.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 8% | 3% |
| 2 | 6% | 4% |
| 3 | 13% | 17% |
| 4 | 15% | 22% |
| 5 - Very important | 53% | 51% |
Figure 79 - A formal written document, completed by the patient, outlining the request.
Why?
This provides a record and evidence of the decision, not only to ensure that it is within the scope of the law but also to highlight how serious it is.

Among the Public, French-speaking participants, women and residents of AB, QC and NL were generally more likely to find this to be very important, along with religious leaders, care or support workers and nurses.
Among the Sample, women and Canadians between 65 and 74 were more likely than others to find this important.
Figure 79 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying? A formal written document, completed by the patient, outlining the request. Pop-up box "Why?": This provides a record and evidence of the decision, not only to ensure that it is within the scope of the law but also to highlight how serious it is.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 5% | 2% |
| 2 | 3% | 4% |
| 3 | 8% | 12% |
| 4 | 14% | 21% |
| 5 - Very important | 62% | 58% |
Figure 80 - The presence of an impartial individual to witness the signing of the written request.
Why?
This could help ensure that the request truly reflects the patient’s wishes, and not that of anyone else.

Among the Public, women and residents of AB were generally more likely to find this to be very important, along with religious leaders, care or support workers and nurses.
Among the Sample, women and Canadians between 65 and 74 were more likely than others to find this important.
Figure 80 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying? The presence of an impartial individual to witness the signing of the written request. Pop-up box "Why?": This could help ensure that the request truly reflects the patient's wishes, and not that of anyone else.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 5% | 3% |
| 2 | 3% | 3% |
| 3 | 7% | 10% |
| 4 | 13% | 21% |
| 5 - Very important | 65% | 61% |
Figure 81 - A repeated number of requests made by the patient.
Why?
This could help ensure the request is both consistent and considered by the patient.

Among the Public, women, Canadians under 35 and between 75 and 84, and residents of AB and MB were generally more likely to find this to be very important, along with religious leaders, care or support workers and physicians.
Among the Sample, English-speaking participants, women and Canadians between 65 and 74 were more likely than others to find this important.
Figure 81 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying? A repeated number of requests made by the patient. Pop-up box "Why?": This could help ensure the request is both consistent and considered by the patient.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 17% | 9% |
| 2 | 9% | 9% |
| 3 | 14% | 21% |
| 4 | 13% | 23% |
| 5 - Very important | 40% | 35% |
Figure 82 - A time delay between requests.
Why?
This could also ensure the request is both consistent and considered by the patient, meeting the Court’s requirement of “enduring suffering.”

Among the Public, women, Canadians under 35 and between 75 and 84, and residents of AB and MB were generally more likely to find this to be very important, along with religious leaders, care or support workers and physicians.
Among the Sample, English-speaking participants and Canadians between 65 and 74 were more likely than others to find this important.
Figure 82 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying? A time delay between requests. Pop-up box "Why?": This could also ensure the request is both consistent and considered by the patient, meeting the Court's requirement of "enduring suffering."
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 15% | 7% |
| 2 | 9% | 5% |
| 3 | 15% | 21% |
| 4 | 13% | 24% |
| 5 - Very important | 41% | 39% |
Figure 83 - A consultation with the patient’s family.
Why?
This could help a physician assess whether the request truly reflects patients’ wishes and values, and whether they are being influenced by a family member.

Among the Public, women, Canadians under 25 and between 75 and 84, and residents of AB and MB were generally more likely to find this to be very important, along with religious leaders and care or support workers.
Among the Sample, women and Canadians between 65 and 84 were more likely than others to find this important.
Figure 83 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying? A consultation with the patient's family. Pop-up box "Why?": This could help a physician assess whether the request truly reflects patients' wishes and values, and whether they are being influenced by a family member.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 13% | 5% |
| 2 | 8% | 6% |
| 3 | 13% | 17% |
| 4 | 13% | 22% |
| 5 - Very important | 46% | 47% |
Figure 84 - A consultation with a mental health professional.
Why?
This could help assess whether the request is being influenced by a treatable mental illness and how clearly the patient was thinking when they made their request.

Among the Public, women, Canadians under 45, and residents of AB and MB were generally more likely to find this to be very important, along with religious leaders, care or support workers and nurses.
Among the Sample, women and English-speaking participants were more likely than others to find this important.
Figure 84 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying? A consultation with a mental health professional. Pop-up box "Why?": This could help assess whether the request is being influenced by a treatable mental illness and how clearly the patient was thinking when they made their request.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 9% | 3% |
| 2 | 6% | 3% |
| 3 | 12% | 12% |
| 4 | 14% | 23% |
| 5 - Very important | 52% | 56% |
Figure 85 - Requests are evaluated by a group of diverse professionals (e.g. doctors, lawyers, social workers).
Why?
This could help reduce the risk of individual bias in determining consent and capacity, and ensure that diverse perspectives are taken into account on behalf of the patient.

Among the Public, women, Canadians under 35, and residents of AB, SK and MB were generally more likely to find this to be very important, along with most professions besides lawyers.
Among the Sample, women and Canadians between 75 and 84 were more likely than others to find this important.
Figure 85 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying? Requests are evaluated by a group of diverse professionals (e.g. doctors, lawyers, social workers). Pop-up box "Why?": This could help reduce the risk of individual bias in determining consent and capacity, and ensure that diverse perspectives are taken into account on behalf of the patient.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 18% | 7% |
| 2 | 9% | 8% |
| 3 | 12% | 19% |
| 4 | 13% | 22% |
| 5 - Very important | 42% | 41% |
Figure 86 - The presence of a physician to observe the patient taking the lethal medication.

Among the Public, French-speaking participants, women, Canadians under 35 and over 75, and residents of QC and NL were generally more likely to find this to be very important, along with religious leaders and care or support workers.
Among the Sample, responses were relatively consistent across demographic groups.
Figure 86 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying? The presence of a physician to observe the patient taking the lethal medication.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 16% | 4% |
| 2 | 7% | 5% |
| 3 | 13% | 14% |
| 4 | 12% | 20% |
| 5 - Very important | 41% | 53% |
Figure 87 - Reporting requirements for physicians for assisted dying requests that are granted or denied.

Among the Public, women and Canadians between 25 and 34 were generally more likely to find this to be very important.
Among the Sample, women and Canadians between 55 and 84 were more likely than others to find this important.
Figure 87 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be required by law before a patient may receive assisted dying? Reporting requirements for physicians for assisted dying requests that are granted or denied.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 4% | 2% |
| 2 | 2% | 2% |
| 3 | 7% | 11% |
| 4 | 13% | 21% |
| 5 - Very important | 66% | 60% |
Safeguards for Physicians
Figure 88 - How important do you think it is to create an external mechanism or process to establish that the legal requirements for assisted dying are met before a request is granted?
Why?
This can help shield physicians from criminal responsibility or civil liability and ensure that professionals with the appropriate expertise are making these decisions.

Among the Public, French-speaking participants, women, Canadians between 55 and 74, and residents of BC, NB and NS were generally more likely to find this to be very important, along with social workers.
Among the Sample, French-speaking participants, Canadians between 55 and 74, and residents of QC were more likely to find this important.
Figure 88 - Text equivalent
Graph charting responses to the following question: How important do you think it is to create an external mechanism or process to establish that the legal requirements for assisted dying are met before a request is granted? Pop-up box "Why?": This can help shield physicians from criminal responsibility or civil liability and ensure that professionals with the appropriate expertise are making these decisions.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 31% | 11% |
| 2 | 3% | 4% |
| 3 | 5% | 15% |
| 4 | 6% | 19% |
| 5 - Very important | 53% | 48% |
Figure 89 - Do you agree or disagree that physicians who refuse to provide assisted dying should be required to provide referrals to other physicians who are willing to provide assistance?

Among the Public, women, Canadians under 35, and residents of AB, MB and NL were generally the most likely to agree, along with religious leaders, physicians, nurses and care or support workers.
Among the Sample, women and Canadians between 65 and 74 were more likely than others to agree.
Figure 89- Text equivalent
Graph charting responses to the following question: Do you agree or disagree that physicians who refuse to provide assisted dying should be required to provide referrals to other physicians who are willing to provide assistance?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 6% | 3% |
| 2 | 4% | 3% |
| 3 | 8% | 11% |
| 4 | 14% | 25% |
| 5 - Strongly agree | 59% | 54% |
Safeguards for Society
How important do you think it is for the following safeguards to be in place?
Figure 90 - Public awareness / education campaign on end-of-life options.
Why?
This could help make people aware of their end-of-life options, as well as the rights and responsibilities of both patients and health care providers.

Among the Public, English-speaking participants, women, Canadians between 55 and 84, and residents of ON were generally more likely to find this to be very important, along with social workers and nurses.
Among the Sample, women and Canadians between 55 and 84 were more likely than others to find this important.
Figure 90 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be in place? Public awareness / education campaign on end-of-life options. Pop-up box "Why?": This could help make people aware of their end-of-life options, as well as the rights and responsibilities of both patients and health care providers.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 6% | 4% |
| 2 | 3% | 5% |
| 3 | 9% | 14% |
| 4 | 14% | 25% |
| 5 - Very important | 62% | 49% |
Figure 91 - Ongoing and mandatory collection, analysis and evaluation of all information pertaining to physician-assisted dying.
Why?
This could help capture important information, highlight key issues, and enable analysis of social trends or patterns revealing possible impact on vulnerable populations or health care delivery.

Among the Public, English-speaking participants, women and Canadians between 25 and 34 were generally more likely to find this to be very important, along with physicians, nurses, care or support workers and religious leaders.
Among the Sample, women, English-speaking participants, and Canadians between 65 and 84 were more likely to find this important.
Figure 91 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be in place? Ongoing and mandatory collection, analysis and evaluation of all information pertaining to physician-assisted dying. Pop-up box "Why?": This could help capture important information, highlight key issues, and enable analysis of social trends or patterns revealing possible impact on vulnerable populations or health care delivery.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 4% | 2% |
| 2 | 2% | 3% |
| 3 | 8% | 13% |
| 4 | 14% | 26% |
| 5 - Very important | 66% | 52% |
Figure 92 - A national oversight body for physician-assisted dying.
Why?
This could help determine if policies are being carried out in compliance with regulations, to conduct research for public reporting, and provide evidence for adjusting or refining policies and regulations.

Among the Public, English-speaking participants, women, Canadians between 25 and 34, and residents of AB, MB and NL were generally more likely to find this to be very important, along with physicians, nurses, care or support workers and religious leaders.
Among the Sample, women, English-speaking participants, and Canadians between 65 and 84 were more likely to find this important.
Figure 92 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be in place? A national oversight body for physician-assisted dying. Pop-up box "Why?": This could help determine if policies are being carried out in compliance with regulations, to conduct research for public reporting, and provide evidence for adjusting or refining policies and regulations.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 8% | 4% |
| 2 | 5% | 4% |
| 3 | 11% | 16% |
| 4 | 14% | 24% |
| 5 - Very important | 56% | 48% |
Figure 93 - A national strategy on palliative and end-of-life care.
Why?
This could help address inequities, such as lack of access and availability of palliative care options for patients who could benefit from this approach.

Among the Public, English-speaking participants, women, Canadians between 25 and 34, and residents of MB and ON were generally more likely to find this to be very important, along with physicians, nurses, social workers, care or support workers and religious leaders.
Among the Sample, women and Canadians between 55 and 84 were more likely than others to find this important.
Figure 93 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be in place? A national strategy on palliative and end-of-life care. Pop-up box "Why?": This could help address inequities, such as lack of access and availability of palliative care options for patients who could benefit from this approach.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 4% | 3% |
| 2 | 2% | 4% |
| 3 | 7% | 14% |
| 4 | 12% | 23% |
| 5 - Very important | 72% | 53% |
Figure 94 - Education for all health care providers around palliative care.
Why?
To ensure health care providers are adequately trained to address patient pain and suffering.

Among the Public, English-speaking participants, women, and residents of MB were generally more likely to find this to be very important, along with nurses, social workers, care or support workers and religious leaders.
Among the Sample, women, English-speaking participants and Canadians between 55 and 74 were more likely to find this important.
Figure 94 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be in place? Education for all health care providers around palliative care. Pop-up box "Why?": To ensure health care providers are adequately trained to address patient pain and suffering.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 2% | 2% |
| 2 | 2% | 2% |
| 3 | 5% | 10% |
| 4 | 11% | 22% |
| 5 - Very important | 79% | 62% |
Figure 95 - A comprehensive national home care strategy.
Why?
To help support people living with disability and advancing chronic illness receive the supports they need to live at home.

Among the Public, English-speaking participants, women, Canadians between 55 and 74, and residents of MB and ON were generally more likely to find this to be very important, along with nurses, physicians, social workers, care or support workers and religious leaders.
Among the Sample, women, English-speaking participants and Canadians between 55 and 84 were more likely to find this important.
Figure 95 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be in place? A comprehensive national home care strategy. Pop-up box "Why?": To help support people living with disability and advancing chronic illness receive the supports they need to live at home.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 3% | 2% |
| 2 | 2% | 3% |
| 3 | 6% | 14% |
| 4 | 11% | 23% |
| 5 - Very important | 75% | 55% |
Figure 96 - A national strategy on disability supports.
Why?
To ensure that appropriate resources are committed to accommodating the needs of people with disabilities, mental illness and chronic health conditions.

Among the Public, English-speaking participants and women were generally more likely to find this to be very important, along with nurses, social workers, care or support workers and religious leaders.
Among the Sample, women, English-speaking participants and Canadians between 55 and 84 were more likely to find this important.
Figure 96 - Text equivalent
Graph charting responses to the following question: How important do you think it is for the following safeguards to be in place? A national strategy on disability supports. Pop-up box "Why?": To ensure that appropriate resources are committed to accommodating the needs of people with disabilities, mental illness and chronic health conditions.
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Not important | 3% | 2% |
| 2 | 2% | 3% |
| 3 | 6% | 12% |
| 4 | 12% | 24% |
| 5 - Very important | 75% | 56% |
Safeguards
Figure 97 - Below are the five safeguards Public participants believed were the most important, on average:

Note: Three of the five safeguards listed above (1, 2 and 5) were among the five most important safeguards for Sample participants (next slide) as well.
Figure 97 - Text equivalent
Graph charting the five safeguards public participants believed were the most important, on average:
| 4 Important | 5 Very Important |
|
|---|---|---|
| Education for all health care providers around palliative care | 11% | 79% |
| Patients understand and appreciate all palliative and medical care options or supports and services that might address a patient’s suffering | 7% | 83% |
| A national strategy on disability supports | 12% | 75% |
| A comprehensive national home care strategy | 11% | 75% |
| Extensive discussion with the patient’s physician | 7% | 80% |
Figure 98 - Below are the five safeguards Sample participants believed were the most important, on average:
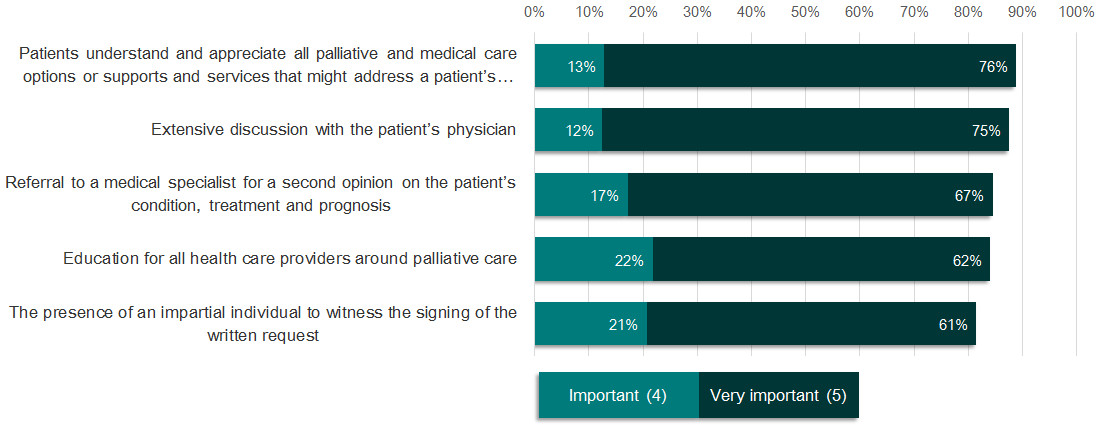
Figure 98 - Text equivalent
Graph charting the five safeguards sample participants believed were the most important, on average:
| 4 Important | 5 Very Important | |
|---|---|---|
| Patients understand and appreciate all palliative and medical care options or supports and services that might address a patient’s suffering | 13% | 76% |
| Extensive discussion with the patient’s physician | 12% | 75% |
| Referral to a medical specialist for a second opinion on the patient’s condition, treatment and prognosis | 17% | 67% |
| Education for all health care providers around palliative care | 22% | 62% |
| The presence of an impartial individual to witness the signing of the written request | 21% | 61% |
Figure 99 - Below are the five safeguards Public participants believed were the least important, on average:

Note: Four of the five safeguards listed above (2-5) were among the five least important safeguards for Sample participants (next slide) as well.
Figure 99 - Text equivalent
Graph charting five safeguards public participants believed were the least important, on average:
| 2 Slightly Important | 1 Not at all important | |
|---|---|---|
| The presence of a physician to observe the patient taking the lethal medication | 7% | 16% |
| A repeated number of requests made by the patient | 9% | 17% |
| Requests are evaluated by a group of diverse professionals | 9% | 18% |
| A time delay between requests | 9% | 15% |
| A consultation with the patient’s family | 8% | 13% |
Figure 100 - Below are the five safeguards Sample participants believed were the least important, on average:

Figure 100 - Text equivalent
Graph charting the five safeguards sample participants believed were the least important, on average:
| 2 Slightly Important | 1 Not at all important | |
|---|---|---|
| A repeated number of requests made by the patient | 9% | 9% |
| A time delay between requests | 5% | 7% |
| Requests are evaluated by a group of diverse professionals | 8% | 7% |
| A consultation with the patient’s family | 6% | 5% |
| A national oversight body for physician-assisted dying | 4% | 4% |
Qualitative Feedback on Additional Safeguards
Summary of responses and sampling of quotes grouped by theme for Issue Book question:
- Are there any additional safeguards for physician-assisted dying that have not been raised? If so, please describe below.
Theme 1: Broad Supports and Alternatives
- Summary:
-
Another important theme that emerged was the identification of broad supports and alternatives which might reduce the demand for physician-assisted dying or turn to this as a last option. Both Open Public and Representative Sample respondents highlighted that there is no reason for a person to suffer either physically or mentally because effective alternatives exist to support living or end-of-life care which is dignified, painless and natural. Palliative care was seen by both groups of respondents as a clear alternative to assisted dying with its focus on the primary goal of optimizing quality of life and helping persons with advanced, progressive, life-threatening illnesses to live as well as possible until they die. Investment in broader societal supports e.g. poverty reduction were also seen by respondents as going a long way to reduce the number of requests for assisted dying.
In the view of many, Canada should develop and/or implement national strategies which support the investment in, and assurance of, available/accessible programs, services and health care providers. Areas for investment include: end-of-life care, palliative, hospice or home care; pain control; mental health treatment and recovery; disability benefits; and, long-term and elderly care. These alternatives were noted to offer a “holistic healthcare system approach” which should be invested in together to offer a full range of options and choice. It is important to note that while some respondents saw assisted dying as “one piece” of this range of options or as a “last resort” others expressed that “assisted suicide and euthanasia should not be presented as or perceived as health care acts or medical interventions, so the providers of these actions should not overlap with health care services.”
Other coping strategies for stress reduction, pain relief and suffering that were identified by respondents of the Issue Book included: faith-based alternatives which shift “social consciousness toward acceptance of death as inevitable and not something to fear”, collaboration with allied health care providers i.e. music therapy, traditional Chinese medicine and Ayurveda.
- Quotes:
-
“We could go a long way toward reducing the number of requests if we as a nation did much better at reducing income inequality, and improving supports for disabled persons and their caretakers, mental health services, end-of-life-care and food security. We have been ignoring many of the things that make life worth living, and I and many I know would be more than happy to pay more in taxes to achieve a civil society in which everyone can live with dignity.”
(Open Public Respondent)“An independent, ongoing review of the availability and funding of programs such as home care, palliative care, counseling [mental health], health care generally, and others I likely haven't thought of, the absence or reduction of which might tend in and of themselves to increase consideration of physician-assisted suicide.”
(Open Public Respondent)“Educate people on the variety of care options and alternatives to physician-assisted dying. Make supports easy to find and access.”
(Representative Sample Respondent)“More free access to specialized services: psychologists, social workers, occupational therapists. Unfortunately, with the austerity and lack of compassion for others, I do not feel that this will open the doors to the well-being of patients.”
(Open Public Respondent in French)“Any and all options need to be implemented around giving every individual the help, support, and information that they need so that they do not feel hopeless. Our true goal as a society should be working toward a reality when there would be no one who would want assistance in dying, because they feel fulfilled, wanted, and worthy of the life they are currently living, regardless of disease or condition.”
(Open Public Respondent)
Theme 2: Minimal or No Safeguards Needed
- Summary:
-
Some Open Public respondents expressed the view that safeguards are either not needed (e.g. Supreme Court has made its ruling and now we need to “move on”) or should be minimal because too many safeguards will ultimately prevent access, impede a timely process, or not respect patient wishes. Representative Sample respondents did not express any explicit views in this area.
Some respondents expressed a differing viewpoint concerning the identification of safeguards stating that many of those listed are not actually safeguards but rather should already be in place as necessary parts of the Canadian health care system and independent of regulations that will permit physician-assisted dying e.g. “having good national policies on palliative care and support for people with disabilities is just good health care policy.”
- Quotes:
-
“A lot of the items on the previous screens just add incredible delay for people who are suffering incredible physical and mental anguish. A national policy on anything takes decades. Referrals to another physician (GP or Specialist) takes months! Let us start with the basis that people know their physical and mental capacity for pain and suffering. It a person wants to go, let them go.”
(Open Public Respondent)“I believe that strong safeguards must be in place but that they must not be so onerous and time consuming that they serve to delay and put in place so many bureaucratic hurdles that it makes the process too difficult and dissuades the person from pursuing this path or seeking out information. There must be a FAIR balance.”
(Open Public Respondent)“As I understand the Supreme Court's ruling, citizens must have the right to make the choice to die. Presently, individuals and their families have been denied this right by the safeguards put in place by people who wish to protect themselves professionally and legally. It is time to safeguard the right for Canadian citizens to make this choice without interference.”
(Open Public Respondent)“By introducing legal roadblocks the patient's suffering will be increased. The less lawyers are involved with PAD the better. Similarly over sight committees will add a significant additional level of bureaucracy and time delay to a decision that should be the patient's alone, in consultation with a medical professional. The power should remain with the patient.”
(Open Public Respondent)“No, everything is clearly mentioned and ultimately, the patient should have the right to decide on the end of their life if they do not want to suffer physically and psychological and if there is no acceptable quality of life.”
(Open Public Respondent in French)
Theme 3: Opposition to Assisted Dying
- Summary:
-
In response to the identification of additional safeguards, a prominent theme which emerged was opposition to assisted dying. Those who were strongly opposed to assisted dying in the Open Public and Representative Samples felt that no safeguards can be put in place to deem this practice acceptable; thus, it should be criminally prohibited with some going as far as counting it as murder.
Opposition to assisted dying is rooted within the following viewpoints:
- Beliefs and Religion: assisted dying was identified by some respondents as an “immoral practice” which goes against one’s basic beliefs of “thou shall not kill” with many emphasizing that only God has the right to end a human life and death is a process which should end naturally.
“All the paperwork and legislation in the world will not make physician assisted dying any safer. God is the giver and taker of life. He gives us suffering on this earth to cause us to trust in Jesus for the grace to live each day here. God can also perform miracles and heal people through the power of prayer. The only guidelines that are applicable in this case are in the Bible.”
(Open Public Respondent)“The best safeguard is for people to be read in the Bible, and recognize that this is only for God to decide.”
(Representative Sample Respondent)
- Relaxing of Eligibility Criteria: this was based on the belief that over time the practice will become more common leading to unintended changes within our health care system and society at large in how we view care options and value human life - “once the line has been crossed, all the safeguards that may be put in place will be subject to constant change and challenge.”
Respondents cautioned of a 'slippery slope' some claim has been experienced in other jurisdictions e.g. Netherlands and Belgium. In particular, respondents were concerned of potential abuses occurring in spite of safeguards - unreported euthanasia deaths, euthanasia carried out without consent, new-born infants born with disabilities euthanized, and obtaining euthanasia without any chronic illness.“Safeguards are only as good as the degree to which they are implemented and enforced. Over time, the acceptance of physician assisted suicide will result in its general acceptance as the norm and the safeguards will slip down the slippery slope.”
(Open Public Respondent)“Normalizing assisted death as a solution for end-of-life issues will create a societal expectation that this is an option that should be considered. This will inevitably create a pressure on patients to consider this option, especially where they or their family feels that the care required will be a burden.”
(Open Public Respondent)“Our whole society is going to change with a mindset to end it all if they are depressed, terminal or not pain controlled. Our society will shift from supporting each other at the time of mental illness, terminal disease or pain to solving these dilemmas by getting a doctor to assist in suicide. What a sad way to look at troubles in our life! We need to build community!”
(Open Public Respondent)
- Protection of the Vulnerable: tied to concerns of relaxing eligibility criteria was the belief that safeguards are not enough to protect and prevent harm to those who are most vulnerable in our society – poor, marginalized, disabled and elderly.
“Safeguards mean nothing when one group of powerful individuals (i.e. doctors, family members) are empowered by legislation to kill vulnerable patients. Safeguards do not prevent abuse of the vulnerable. They just make us feel better that we did everything we could when the abuse happens. It's better to say no to all abuse than to let some vulnerable patients slip through the cracks and be killed.”
(Open Public Respondent)“The main goal here is to prevent the most vulnerable people from harm. Prohibiting euthanasia is the best way. If not, make restrictions tight and have a judicial review very regularly to make sure the law is being followed in the assisted deaths.”
(Open Public Respondent)
- Erosion of Medical Ethics: lastly, arguments against assisted dying were rooted in concerns over asking doctors, nurses or any other health care professionals to engage in activities which would be a violation of fundamental medical ethics and the Hippocratic Oath to cure patients and would therefore “ruin” him or her for the care of others.
"Safeguards are only as good as the degree to which they are implemented and enforced. Over time, the acceptance of physician-assisted suicide will result in its general acceptance as the norm and the safeguards will slip down the slippery slope.”
(Open Public Respondent)“Physicians are not executioners. Their purpose is to promote health and to heal. They should never be put into a position that they have to execute an individual or recommend and executioner to them.”
(Open Public Respondent)
- Broad Supports and Alternatives: Both groups signaled the importance of practicing comfort and treatments which do not include assistance in ending someone's life.
- Beliefs and Religion: assisted dying was identified by some respondents as an “immoral practice” which goes against one’s basic beliefs of “thou shall not kill” with many emphasizing that only God has the right to end a human life and death is a process which should end naturally.
Theme 4: Participation and Referral - Unforced
- Summary:
-
According to many Open Public respondents it is important to ‘protect freedom of conscience’ of all medical and health workers (doctors, nurses, pharmacists). Respondents felt they should not be forced to participate in practices (i.e. assisted dying) which go against their medical ethics but also moral or religious beliefs. This viewpoint was held similarly by a few Representative Sample respondents.
Many noted that physicians should be under no obligation to refer patients to a physician who is willing to conduct this practice rather it was suggested that a self-referral system be implemented to avoid putting the ‘burden’ on the physician to refer. Through this system it was suggested that patients could conduct their own online search or visit a center that provides the names of doctors providing service in their community. Physicians who feel they cannot participate in assisted suicide, need to be supported in their decision free from any legal ramifications (fines or penalties) or discrimination in particular as it relates to job security.
A suggested alternative to participation and referral includes developing a new professional class with the role of assisting with dying and suicide. This alternative helps to “put doctors who are against assisted suicide out of the picture”; however, the exception is that they need to refer a patient to one of these professionals upon request. This new profession would be trained to ensure proper requirements and techniques are employed, just as current professionals such as engineers, doctors, lawyers do…
- Quotes:
-
“All doctors and health care workers should be able to live by their conscience. We need them. They should NOT have to refer patients for euthanasia if it is against their conscience or religion.”
(Open Public Respondent)“Explicitly protect the conscience rights of all physicians and health care workers so they have the freedom to refuse to take part in, refer for, or counsel against the killing of any patient. No other jurisdiction that allows euthanasia or assisted suicide imposes a legal duty on physicians who conscientiously object to make referrals for physician assisted death.”
(Open Public Respondent)“Absolute freedom in all provinces and jurisdictions with no reprisals for Doctors who because of conscious objection who will not refer or participate in euthanasia. I see too much in our country of people being forced to live and work outside of their beliefs or conscience.”
(Open Public Respondent)“There is considerable risk to the wellbeing of health care providers involved in the provision of this ‘service’. This cannot be a required action in the registration of health care providers or not many of the people you want to attract to this profession will apply. This is not something many health care providers would be comfortable with. It is still a service that is very appropriate within the Canadian health care system, and very much needed to be provided in the correct circumstances.”
(Representative Sample Respondent)“The requirement on the physician is unreasonable because their oath was to preserve life, this changes their profession and it may become an issue to have fewer doctors. We run a risk of changing and losing valuable physicians to a death cultured breed of physician. I personally will lose faith in the professionals.”
(Open Public Respondent)
Theme 5: Patient Choice / Right to Die
- Summary:
-
The view that people should have freedom of choice, including the right to control their own body and life, not prolong suffering, and be free from outside influence, was expressed predominantly by Open Public respondents. It was suggested that after considering the information and issues that affect them and their family, patients should have the right to choose physician-assisted dying. Both groups of respondents expressed the belief that with that choice should come the choice as well to change one’s mind. Others maintained that a patient’s wish to die should be protected, provided they meet the conditions laid down by the Supreme Court.
- Quotes:
-
“I believe that the only person who should be able to make the final decision should be the person whose life is in question. I believe that a doctor can offer life ending options but should never be allowed to make the final decision for the patient, regardless of metal or physical condition.”
(Open Public Respondent)“Although decisions should be carefully weighed and follow a defined process, the 'agreement' of a diverse committee on each end-of-life decision threatens to once again remove the autonomy and dignity of the patient. Patients are making a very difficult decision, which should be made with the assistance of their physician and mental health professionals, and should be respected. At no point should they be requesting 'permission' from an external body.”
(Open Public Respondent)“This should be the right of persons to control and have a say in end of life decisions. That kind of autonomy can only be served by appreciating that most persons would choose life but in situations where it has become unbearable there are ways to be able to end one's life without having to leave your home or Country or suffer by refusing treatment.”
(Open Public Respondent)“Everyone will have a different threshold for what they define as the "tipping point" I believe this must be considered and respected. Physicians must learn to respect and uphold the patients wishes.”
(Open Public Respondent)“There must be an easily accessible, always available, none punitive and simple mechanism whereby the patient can change his or her mind regarding any request to terminate his or her life at any point in time right up to the final moment. In other words, a person should have the right and ability to change their mind right up until it is too late to do so.”
(Representative Sample Respondent)“NO pressure from family or caregivers should be experienced when making such a personal decision to end their life. DOCTORS should be making referrals for their patient if they REFUSE to participate, its the patients request.”
(Open Public Respondent)“Once the patient has made their decision and it is deemed reasonable and undertaken with full knowledge, the next of kin should not be allowed to interfere. It is my understanding that currently next of kin can override a patient's wish to be an organ donor. This is wrong and it should not be allowed in end-of-life situations.”
(Open Public Respondent)“Safeguards need to be introduced to ensure that access is not denied to any competent adult who is suffering in a manner which is unacceptable to THEM. It doesn't have to be unacceptable to a psychologist, a doctor, their family, or any other person. You cannot judge for somebody else.”
(Open Public Respondent)“The ability to die should be a choice of the individual, after that individual is informed of their options and still chooses to die. Assisted dying should NEVER be a decision that a committee of professionals needs to approve.”
(Open Public Respondent)“The most significant safeguard that we need to consider is to create a system that safeguards the patient's expressed wish to die, provided they meet the conditions laid down by the Supreme Court. This fundamental right must not be subverted by inaccessible, bureaucratic systems created to appease concerns of the medical profession and religious groups.”
(Open Public Respondent)
Theme 6: Review and Oversight
- Summary:
-
In sharing their views on how to mitigate perceived risks and harm of physician-assisted dying for those most vulnerable, respondents identified processes or entities that would provide a review or oversight function before physician-assisted suicide could be provided. It was also suggested that review or oversight should take place afterwards for monitoring and evaluation purposes.
Key processes for review and oversight suggested by respondents of the Issue Book included requiring:
- Counselling: physicians refer patients that may be suffering from psychiatric or psychological disorders or depression for counselling. Death may not be granted until it can be confirmed by the counsellor that the patient is not suffering psychologically or from depression.
- Consent: It was suggested that consent be witnessed by at least two others (one of the witnesses must not be a relative or someone entitled to a portion of their estate), with the entire process video recorded from beginning of request, discussion with doctors, panel hearings, lethal injection and pronouncement of death. These video's must be regularly and independently reviewed by a joint panel of doctors, lawyers and ethicists and must be immediately and full accessibly to any judge, officer of the court or Parliamentarian upon request.
It was also noted that consent must be given both orally and written, no less than 15 days apart, and can be rescinded at any time and in any manner without regard to his or her mental state. While it is important that we have a formal, written process in order to document a request by a patient to end their life, it must not be designed in such a way as to cause an impedance to any individual who seeks to end their life - for example, people with low literacy or language barriers or those who have suffered a severe stroke. As such, all efforts must be made to ensure the process is as inclusive as possible, including providing alternate forms of documentation to those patients who are incapable of physically writing a request (video, sign language). Conversely, many people who are capable of clearly communicating their wish to die may be intimidated by the task of writing a formal request and may not have experience writing formal documents themselves. Therefore, it was suggested that or providing resources to allow these individuals to write a request without relying on the help of friends/family who might influence them. - Validation: It was suggested that the onus must be on those who are involved in administering physician-assisted dying to provide evidence from third parties that the request for death is not coerced, in every case. Failure to provide this should result in sanctions and other repercussions potentially including criminal charges.
As a mechanism to support ongoing monitoring, Open Public respondents overwhelmingly identified the need for a judicial review every three years of all assisted suicide deaths. Should it be found that the law is not being followed it was suggested that an immediate moratorium of all assisted deaths be put in place and not lifted until the law can be amended to fully prevent harm.
It was also widely suggested that an agency be created (reporting to the Minister of Justice or be formed through the Canadian Medical Societies/Association) with the mandate of monitoring assisted suicide deaths to ensure the law is being followed. A "Center of Excellence" approach was suggested to provide better control nationally to ensure established protocols are consistently applied and would better enable a reliable statistical data bank for evaluation purposes.
Additional or alternative review and oversight processes or entities suggested by respondents of the Issue Book included:
- Audits and Data Reporting: audits should be conducted with severe penalties for anyone who takes or assists in taking a human life without reporting it; public records should also be maintained on who has received assisted dying services or who has aided in this practice, directly or indirectly.
- Ethics Committees: the role of Ethics is paramount in the formulation of policy related to safeguards.
- Review Committees: to oversee and discuss each request submitted by the doctor; this would be a collaborative committee potentially including, physicians, nurses, public, pharmacists, clergy etc. to obtain unbiased evaluation and approval in a timely manner. Such a committee would serve as a support to physicians so that they are not left with the primary decision. The committee should be knowledgeable about the laws as well as medical and moral implications of the decision. There should also be an appeal process for the patient. Patients whose life expectancy is greater than 3-6 months should require a separate and more formal process, including a review board of expertise (legal, medical, ethicists) or hearing.
- Compliance reviews: appointed by an external commission this review would be conducted to ensure that all guidelines are being followed (should be conducted before the death has taken place, rather than afterwards) but this should not impose unreasonable delays - i.e., the review shouldn't add more than a few weeks to the process.
- Random Checks: to ensure all policies by patient and physician are being followed.
- Peer Reviews: for doctors (not Administrators or HR personnel) to evaluate other doctors, in order to establish and informally certify the health and robustness of the presiding doctors’ reasons for engaging in providing assisted-dying services.
- Federal and provincial Ombudsmen: to ensure appropriate and needed legislation and supports are in place.
- Consideration of a cultural and diversity lens in access to physician-assisted dying: issues should also be considered in the process and monitored e.g. Canada already has a disproportionate number of Aboriginal and First Nations people dying by suicide. It would be important to ensure this was not a factor (either way) in access to physician-assisted suicide and therefore any oversight body should include the capacity to monitor with this lens. Consumers/patients/families/citizens should be involved in the design and ongoing monitoring of the process from a purely neutral perspective (i.e. not medical. legal or economic).
Evaluation of Issue Book Questionnaire by Respondents
At the end of each Issue Book, participants were asked to evaluate their experience with the consultation and to provide feedback on how information was presented. The following slides present the results of the participant evaluations.
Key Findings
- Participants indicated they were very satisfied with the consultation process, particularly those from the Representative Sample:
- 90% of Representative Sample respondents and 74% of Open Public respondents agreed that “The information was clearly presented.” (2% of Representative Sample respondents and 9% of Open Public respondents disagreed)
- 87% of Representative Sample respondents and 65% of Open Public respondents agreed that “The information was well balanced between different views on the issue.” (3% of Representative Sample respondents and 16% of Open Public respondents disagreed)
- 83% of Representative Sample respondents and 61% of Open Public respondents agreed that “This online consultation helped you learn about the key issues and concerns.” (3% of Representative Sample respondents and 17% of Open Public respondents disagreed)
Evaluation
Figure 101 - The information was clearly presented

Figure 101 - Text equivalent
Graph charting responses to the following question: The information was clearly presented?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 4% | 1% |
| 2 | 5% | 1% |
| 3 | 15% | 7% |
| 4 | 30% | 27% |
| 5 - Strongly agree | 44% | 63% |
Figure 102 - The information was well balanced between different views on this issue

Figure 102 - Text equivalent
Graph charting responses to the following question: The information was well balanced between different views on this issue?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 7% | 1% |
| 2 | 9% | 2% |
| 3 | 16% | 9% |
| 4 | 26% | 26% |
| 5 - Strongly agree | 39% | 61% |
Figure 103 - This online consultation helped you learn about the key issues and concerns

Figure 103- Text equivalent
Graph charting responses to the following question: This online consultation helped you learn about the key issues and concerns?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 9% | 1% |
| 2 | 8% | 2% |
| 3 | 19% | 11% |
| 4 | 24% | 24% |
| 5 - Strongly agree | 37% | 59% |
Figure 104 - The online consultation provided you with a good opportunity to express your views on this issue

Figure 104 - Text equivalent
Graph charting responses to the following question: The online consultation provided you with a good opportunity to express your views on this issue?
| Open Public Responses | Representative Sample Responses | |
|---|---|---|
| 1 - Strongly disagree | 4% | 1% |
| 2 | 5% | 1% |
| 3 | 14% | 8% |
| 4 | 27% | 24% |
| 5 - Strongly agree | 48% | 64% |
- Date modified: